Read the latest and greatest from our team
of incredible specialists.

Beach House Recovery Center » Blog » Heroin Detox Guide
Although heroin has been feared for two generations as an addictive drug of the worst kind, it originally was marketed as a cure for other opiate addictions. Heroin was first derived from morphine in nineteenth-century Germany. The Bayer Company began selling it in 1898 as a treatment for chronic cough and tuberculosis, among other illnesses. Heroin was also billed as a safe and non-addictive substitute for the morphine that was a serious addiction concern in the post-Civil-War United States. In retrospect, this seems a preview of the contemporary opioid-painkiller epidemic: apparent wonder drug is discovered, prescribed indiscriminately, recognized as dangerous only after damage has been done on a large scale.
Heroin was officially banned in 1924—(it’s now classified as a Schedule I drug with no legitimate medical purpose)—but over 625,000 people in the United States are now addicted to it. Many of these people first became dependent on opiate painkillers, then turned to heroin as a cheaper and easier-to-obtain substitute: from 2002 to 2016, the number of Americans with heroin addiction nearly tripled.

While it’s rare for heroin withdrawal to be actually life-threatening, the symptoms of withdrawal can make you feel terribly sick. These include:

Occasionally, someone experiencing withdrawal will experience convulsions, seizures or hallucinations.
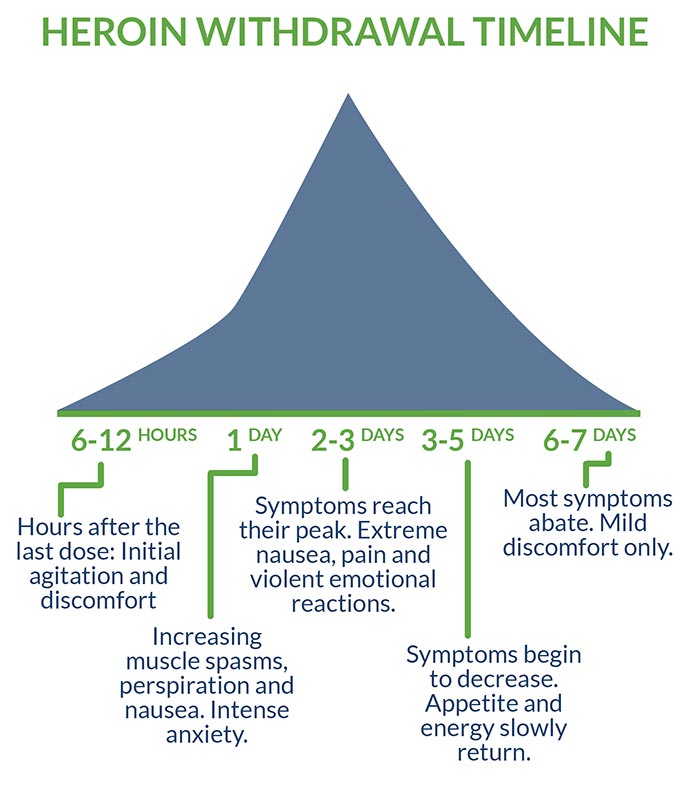
There are other differences in individual experiences of heroin withdrawal, but in most cases, physical withdrawal lasts about a week. Typically, the process goes like this:
Factors that affect intensity and duration of withdrawal include:
Even after physical detox, heroin cravings may recur periodically for several months. For this reason, ideally, three-plus months of follow-up care with daily therapy is recommended to prepare the patient for life without drugs. Getting support during this vulnerable period is an element in most recovery success stories.
Inpatient care, which involves residential hospitalization, is frequently recommended because:
Inpatient care also allows ongoing supervision of anyone receiving Medication-Assisted Treatment to curb cravings. With heroin, there are special concerns here. Alternate opioid drugs, notably methadone, have been routinely used to reduce heroin-relapse cravings for decades, but—reminiscent of heroin’s earlier use in treating morphine addiction—also generate dependence issues of their own. Many former heroin addicts are now re-entering detox centers to get support and help to discontinue methadone, so it’s important that any program using alternate opiates includes a discontinuation plan.
Anyone without a solid support network on the outside almost certainly needs inpatient care. So does anyone living with the stress of a dual diagnosis (a mental illness in addition to the addiction).
For all its advantages, inpatient care isn’t always practical for everyone. The pros of leaving residential treatment may outweigh the cons if someone:
A client whose situation matches that description still needs professional therapy and supervision for the first few months after detox. The solution may then be outpatient treatment, which involves regularly reporting to aftercare facilities. Most outpatient programs are based on one of the following models:
Most people in outpatient situations, especially if living beyond walking distance of the detox center, are more vulnerable to relapse than those in structured and supervised living environments. It’s important to have a detailed relapse-prevention plan, secure family support and arrange accountability for keeping all appointments.
Looking at everything involved in both inpatient and outpatient treatment, many people are tempted to think, “That sounds like an awful lot of trouble. Why can’t I just take a few sick days and quit cold at home?”
For one thing, just because heroin detox rarely kills outright doesn’t mean it’s safe. Some people become dehydrated from nausea and vomiting. Some become so frantic that they attempt suicide. The most likely danger, however, is that someone will yield to relapse cravings, put a fresh dose of heroin into a weakened body, and suffer a lethal overdose.
Even in the best-case scenario—a person has used opiates for a relatively short time, is in overall good health and has trustworthy support on hand—it’s virtually impossible to ensure the level of comfort, care, and safety available from medically supervised inpatient treatment. And even the home-detox success stories remain in significant danger of relapse without professional help to deal with the reasons behind the addiction, and without a support plan for dealing with a recurrence of cravings.
Even in a clinical setting, there are varying opinions on the safest forms of detox. Many clinics opt for the cold turkey approach of cutting off all drugs and simply keeping the client comfortable, rather than risk possible complications from substitute opiates. However, hundreds of programs still opt for methadone to spare body and brain the full shock of heroin withdrawal: more than 356,000 opioid-addiction clients received methadone in 2015. The more preferable alternative to methadone: a short-term course of Suboxone, which increasingly is recognized as the gold standard of care when combined with behavioral therapies.
Treating heroin addiction with Suboxone is a form of tapering, which involves administering gradually reduced doses of a drug (or a safer substitute with similar effects) until a client is weaned from all cravings. Suboxone can be beneficial for patients at high risk for dangerous withdrawal symptoms or relapse. There is, however, real danger that people will treat these drugs simply as heroin substitutes and stay on them indefinitely, so it’s important to continue the tapering-off until a patient is opiate-free.
Once a heroin detox client is clear on preferred medical approach, other factors to consider in choosing a treatment center include:
Heroin rehab can cost hundreds of dollars a day, but even expensive centers are sound investments considering the costs of staying addicted: over $100 a day for the drug, plus damage to health, relationships, property and productivity.
Unfortunately, dangers and potential costs don’t go away after addiction treatment. As with other chronic illnesses, around half of clients will have at least one subsequent relapse. Relapse doesn’t have to mean a return to full addiction, however: the true success stories are those who make ongoing progress and are happily sober in the long term.
Getting support, a vital part of heroin detox is also an important tool in avoiding relapse and in recovering from any relapses that do occur. Clients completing official heroin-addiction treatment are advised to continue with regular support in the forms of:
Over 15,000 people in the United States now die each year from a heroin overdose. Addiction treatment saves lives.
For related information, see the following articles:
AddictionBlog.org. “The Cost of Heroin Addiction.” Retrieved from http://addictionblog.org/infographics/the-cost-of-heroin-addiction-infographic/
Gupta, Dr. Sanjay (2016, June 2). “Unintended Consequences: Why Painkiller Addicts Turn to Heroin.” CNN.com. Retrieved from https://www.cnn.com/2014/08/29/health/gupta-unintended-consequences/
Moghe, Sonia (2016, October 14). “Opioid History: From ‘Wonder Drug’ to Abuse Epidemic.” CNN.com. Retrieved from https://www.cnn.com/2016/05/12/health/opioid-addiction-history/index.html
National Institute on Drug Abuse (2017, September). “Overdose Death Rates.” Retrieved from https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates
National Institute on Drug Abuse (2018, January). “How Effective Is Drug Addiction Treatment?” Retrieved from https://www.drugabuse.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition/frequently-asked-questions/how-effective-drug-addiction-treatment
National Institute on Drug Abuse (2018, June). “What Is the Scope of Heroin Use in the United States?” Retrieved from https://www.drugabuse.gov/publications/research-reports/heroin/scope-heroin-use-in-united-states
Substance Abuse and Mental Health Services Administration (2017, August 22). “SAMHSA Report Shows Increase in Opioid Treatment Facilities.” Retrieved from https://www.samhsa.gov/newsroom/press-announcements/201708220100
United Nations Office on Drugs and Crime (1953, January 1). “History of Heroin.” Retrieved from http://www.unodc.org/unodc/en/data-and-analysis/bulletin/bulletin_1953-01-01_2_page004.html
United States Drug Enforcement Administration. “Drug Scheduling: Drug Schedules.” Retrieved from https://www.dea.gov/druginfo/ds.shtml
U.S. Food and Drug Administration (2018, May 16). “FDA Approves the First Non-Opioid Treatment for Management of Opioid Withdrawal Symptoms in Adults.” Retrieved from https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm607884.htm
Whether you’re researching for yourself or a loved one, Beach House can help. We understand that this is a serious time in your life and that the treatment center you choose matters. We want you to feel comfortable and empowered to make the right decision for yourself, a friend, or a family member. This is why a counselor is waiting and available to answer your questions and help put your mind at ease regarding the next steps. Many of the staff at Beach House have walked in your shoes. If you feel you’re ready or want more information about how to help a loved one, we can help today. You can also learn why we are voted the #1 rehab for addiction treatment in Florida.
We accept most major insurance plans and can verify your benefits quickly and confidentially.
We’re committed to helping you access the care you need, our admissions counselors can guide you through your coverage options and available resources.





"*" indicates required fields