Hydrocodone Detox Guide – Withdrawal & Symptoms
[one-half-first]
Hydrocodone, a pain killer commonly prescribed in combination with acetaminophen, is the most popular opiate (narcotic) available in the US. Hydrocodone abuse is rampant, with illicit distribution and immoderate use spiraling to epidemic proportions. This alarming reality prompted the Drug Enforcement Administration (DEA) to re-classify the drug as a Schedule 11 substance in 2013. In 2016, approximately 46 people died daily from prescription opiate overdoses, which account for over 40% of opiate-related deaths.
Hydrocodone, like other opioids, alters brain chemistry, creating dependency in the process. Opiates work by binding to opiate receptors throughout the central nervous system and brain, functioning as atypical nervous system depressants. This depressant effect impairs multiple bodily functions, including reducing blood pressure, slowing breath and lowering body temperature.
[/one-half-first]
[one-half]
Table of Contents
- Introduction to Hydrocodone Detox
- Hydrocodone Withdrawal Symptoms
- Hydrocodone Withdrawal Timeline
- Inpatient Treatment for Hydrocodone
- Outpatient Treatment for Hydrocodone
- Can Hydrocodone Detox Be Done at Home?
- Tapered vs. Cold Turkey
- Considerations for Hydrocodone Detox
- Recovery Success and Aftercare Services for Hydrocodone
[/one-half][clearfix]
Once opiate-dependent, users require increasing amounts of the drug to achieve the same fleeting, euphoric effect. According to the National Institute on Drug Abuse (NIDA), this dependency negatively impacts every aspect of the user’s life, with social, legal, financial and personal ramifications eventually escalating to a crisis point. Due to hydrocodone’s highly addictive properties, and the resulting physiological changes that accompany chronic use, the majority of users require professional help in order to safely remove the toxic effects of the drug from their system.
Is hydrocodone ruining your life? Call: (855) 935-2871
HYDROCODONE WITHDRAWAL SYMPTOMS
Once someone becomes opiate-dependent, stopping suddenly is dangerous. The resulting acceleration of heart rate, combined with dramatic spikes in blood pressure and body temperature, can turn deadly.
Withdrawal symptoms are assessed upon entry into a hydrocodone detox program using a variety of tools and objective measurements like the Clinical Opiate Withdrawal Scale (COWS). This initial evaluation is critical to effective treatment. The severity of scores dictates when Medication-assisted treatment (MAT) and detox should begin. Depending upon whether or not a client is experiencing early or late-stage symptoms, the effects of hydrocodone withdrawal may include the following:
[one-half-first]
- Anxiety
- Insomnia
- Sweating
- Agitation
- Joint and muscle aches
[/one-half-first]
[one-half]
- Vomiting
- Nausea
- Abdominal cramping
- Dilated pupils
- Goose bumps
[/one-half][clearfix]
HYDROCODONE WITHDRAWAL TIMELINE
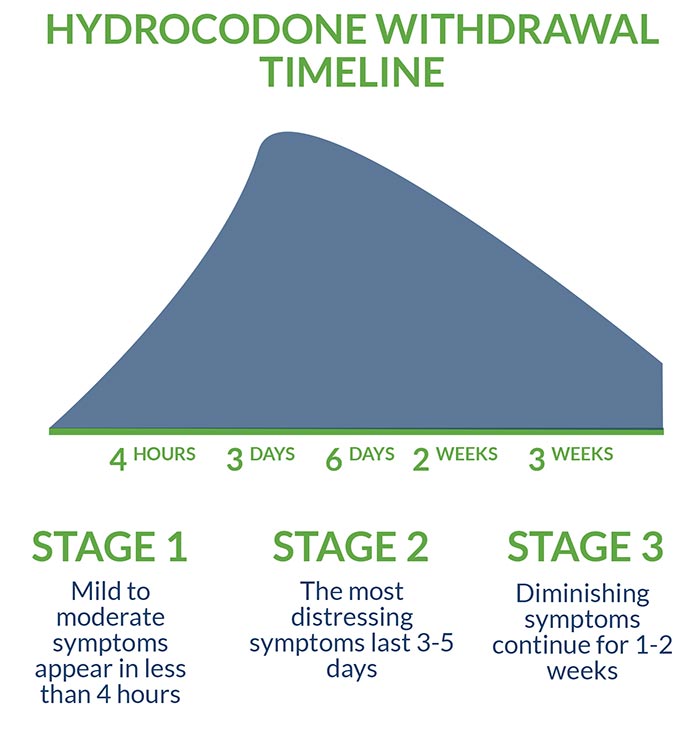
The primary objective of a medically managed hydrocodone detox is to prevent “precipitated withdrawal,” the rapid and unsettlingly intense onset of symptoms. Mild to moderate hydrocodone withdrawal symptoms may appear in as little as four hours following the last dose. The most acute and distressing symptoms last approximately three to five days, while diminishing symptoms continue for approximately one to two weeks.
Although the acute phase of hydrocodone withdrawal typically peaks quickly, the lingering effects of post-acute withdrawal syndrome (PAWS) depend upon a variety of factors such as age, individual biochemistry, ongoing medical treatment and dietary/lifestyle choices. Other factors determining the immediacy, intensity and duration of hydrocodone withdrawal symptoms include whether a client is addicted to short or long-acting opiates, as well as the length, severity and frequency of use. For heavy, chronic users, PAWS symptoms may be experienced for years.
Hydrocodone can typically be detected via urine testing for up to four days following the last dose, whereas blood tests can reliably detect the opiate for only 24 hours. Hair samples provide the longest range of detection, with traces appearing for up to 90 days.
INPATIENT TREATMENT OF HYDROCODONE
While many treatment options exist, intensive inpatient treatment in a residential detox is considered the gold standard. Inpatient treatment includes more comprehensive medical and behavioral health services, with many programs featuring additional holistic benefits. Inpatient treatment also offers the advantage of a safe, supportive, and sober environment in which clients receive 24/7 monitoring, seven days a week, as they move through the stages of withdrawal.
Medication-Assisted Treatment
Medication-assisted treatment (MAT) is the popular protocol in which medications are used in tandem with counseling and behavioral therapy. MAT frequently includes the following evidence-based, Food and Drug Administration (FDA)-approved pharmacological interventions:
- Suboxone provides a controlled, long-lasting dose of opioids without producing the same high as hydrocodone.
- Vivitrol targets the same brain receptors as hydrocodone while blocking the desirable effects.
- Subutex produces a similar but less powerful effect when compared to hydrocodone, which helps reduce withdrawal symptoms and diminish cravings.
Dual Diagnosis Treatment
Depending upon individual client needs and the presence of co-occurring anxiety or depression-related disorders, a variety of other medications including SSRIs, gabapentin, buspirone and pregabalin may be utilized to ensure maximum stabilization and long-term benefit. Post-traumatic stress disorder (PTSD) is frequently a precipitating factor involved in opiate dependence and is included in the scope of “dual diagnosis” treatment.
OUTPATIENT TREATMENT OF HYDROCODONE
Outpatient treatment offers many of the same benefits and services as inpatient treatment on a less comprehensive basis, and without the added precaution of 24-hour monitoring and patient supervision. Popular in a variety of facilities such as hospitals, clinics and doctors’ offices, outpatient treatment offers a degree of flexibility that is preferred by some clients based upon their personal and/or professional needs.
CAN HYDROCODONE DETOX BE DONE AT HOME?
Due to the severity of hydrocodone addiction and potentially dangerous effects, at-home, self-guided hydrocodone detox is never recommended. Only trained medical professionals can determine exact medication requirements and prescribe individualized treatment, while licensed clinicians help identify and resolve the psychological issues associated with addiction through targeted, client-specific therapy. Unmanaged, hydrocodone withdrawal symptoms frequently lead to relapse or less than favorable treatment outcomes.
TAPERED VERSUS COLD TURKEY
Depending upon the sound judgment of a medical professional and individual case history, a tapered approach to hydrocodone detox is frequently utilized, with client safety and a carefully controlled medication regimen remaining a top priority throughout the process. Stopping a highly addictive opiate cold turkey subjects the body to an unnecessarily harsh backlash effect, making the possibility of relapse more likely. For this reason, going cold turkey is never recommended.
CONSIDERATIONS/HOW TO DECIDE WHAT IS RIGHT FOR YOU
Treatment options, locations and affordability are all variable, with no single method or option being preferable in every case. Insurance becomes a major consideration for most clients, and many receive partial, if not total, coverage for services rendered.
Any reputable facility will verify insurance benefits to ensure a relatively smooth, stress-free admission process. In cases where out-of-pocket costs are required, payment plans and options are discussed, as well as the possibility of scholarships and/or federal grants.
Although treatment in a public, institutional setting is readily available, private treatment is considered preferential. The impressive staff-to-client ratio and diversity of treatment modalities help ensure a successful program, while the comprehensive nature of in-house and aftercare services add value to the client’s experience. Though inpatient treatment is generally considered more effective, outpatient treatment offers the cheapest detox service, and, in some cases, the only available option for those with highly demanding personal and/or professional schedules.
RECOVERY SUCCESS AND AFTERCARE SERVICES FOR HYDROCODONE
A diversity of factors ranging from individual motivation and physical health, to family support and personal spirituality, all affect the hydrocodone withdrawal process and treatment outcomes. Attending 12-Step programs such as Narcotics Anonymous (NA) and involvement in other recovery-related communities and activities is critical to long-term sobriety and provides the framework necessary for post-treatment success. Furthermore, a comprehensive aftercare plan that includes random drug testing, medication management, one-on-one and/or group therapy, life and job skills services, a healthy diet and regular physical activity are all part of an empirically proven relapse prevention strategy.
For more about hydrocodone detox and recovery, check out these related articles:
- “Painkillers Explained: Understand What Medicines Doctors are Prescribing for Your Pain and How They Affect You”
- “How Genetic Testing is Being Used to Reduce the Opiate Epidemic”
- “Is Addiction Genetic? How Genetic Predisposition Can Play a Role in Addiction”
Is hydrocodone ruining your life? Get help now
[expand title=" Sources:" targclass="highlight"]
Journal of Pain Research. Extended-Release hydrocodone – gift or curse? Jan 10, 2013.
MSC Addiction Studies. Hydrocodone Detox Symptoms, Timeline, Medications and Treatment. Aug 22, 2015.
Center for Disease Control (CDC). US Drug Overdose Deaths Continue to Rise: Increase Fueled by Synthetic Opioids. March 29, 2018.
National Institute on Drug Abuse (NIDA). Opioid Overdose Crises. March, 2018.
Journal of Opioid Management. Pharmacokinetic Evaluation of Hydrocodone/Acetaminophen for Pain Management. Jan, 2013.
[/expand]