Read the latest and greatest from our team
of incredible specialists.

Beach House Recovery Center » Blog » Methadone Detox – Withdrawal Symptoms and Timeline
Methadone is a synthetic opiate painkiller commonly used to treat individuals suffering from opiate addiction—especially to heroin and prescription painkillers. A long-acting opiate, methadone was originally introduced in the mid-1900s by German scientists as an alternative to morphine. Following the prevalence and success of methadone clinics in the 1970s, its popularity steadily increased. Classified as a Schedule 11, highly regulated narcotic by the Food and Drug Administration (FDA), methadone is often an object of rampant and illicit distribution and diversion.
Methadone’s relatively inexpensive cost compared to other prescription painkillers helps explain its popularity. When compared to opiate pain killers such as hydrocodone and oxycodone, methadone is considered a “preferred drug” by insurance companies in as many as 33 states—a fact responsible for many people changing their prescriptions and unintentionally becoming addicted.

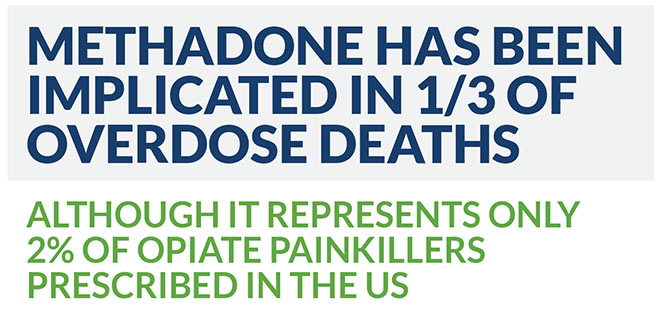 Methadone’s widespread use as a transition drug to help wean users off other opiates, most notably heroin, has created a deadly epidemic prompting calls for greater regulation of the drug:
Methadone’s widespread use as a transition drug to help wean users off other opiates, most notably heroin, has created a deadly epidemic prompting calls for greater regulation of the drug:
Methadone targets the same brain receptors as other opiates. Through a binding process, the drug works to dull the perception of pain, inducing short-term euphoria and setting the stage for addiction. Long-term methadone dependence is dangerous because of the unpredictable interactions and tolerance the drug creates in users—many of whom use other opiates. Even casual recreational use may result in dependency and significant withdrawal symptoms.
Methadone withdrawal requires professional medical evaluation and management. Clients are administered various physical and psychiatric assessments prior to beginning treatment, and specialized tools like the Clinical Opiate Withdrawal Scale (COWS) help determine the severity of symptoms based on scores. The scores obtained during the evaluation then inform medication-assisted treatment (MAT) and determine client-specific therapy. Depending upon the frequency, duration and intensity of use, clients may experience the following cluster of early and late stage withdrawal symptoms:
Methadone’s long-acting properties accumulate quickly in the majority of users and present a unique danger. Unlike other opiates, even taking one additional dose of the drug can result in an overdose or complicate the withdrawal process. This is, in part, explained by methadone’s depressant effect on the heart and lungs—which continues long after its pain-relieving effects have subsided. Methadone has an unusually long and variable half-life of approximately 8-60 hours.
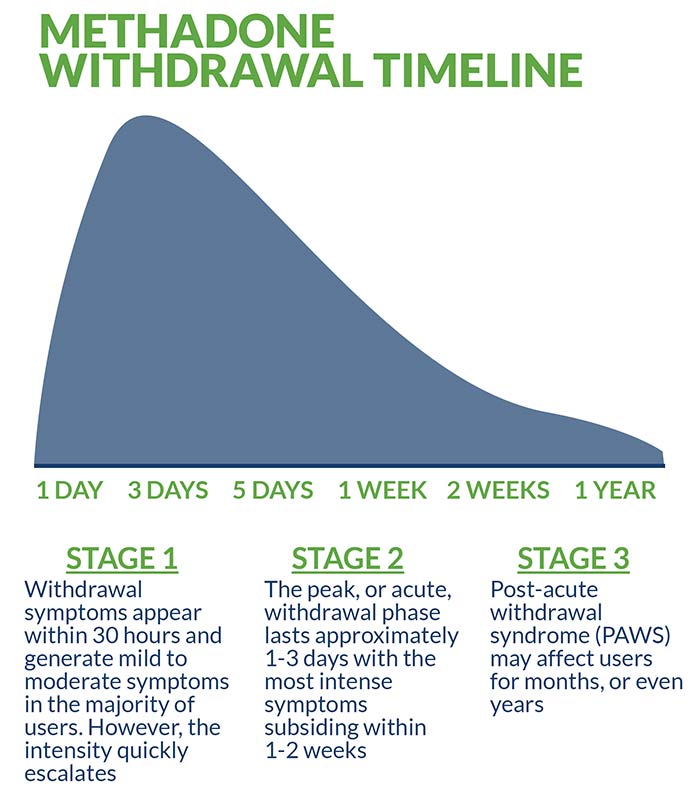
Typically, withdrawal symptoms appear within 30 hours following dosage and generate mild to moderate symptoms in the majority of users. However, the intensity quickly escalates. The peak, or acute, withdrawal phase lasts approximately one to three days with the most intense symptoms subsiding within one to two weeks. The third, and final, stage of methadone withdrawal is known as post-acute withdrawal syndrome (PAWS) and its diminishing effects may impact users for months, or even years. In rare cases, permanent damage is sustained as a result of the drug’s potency and unpredictable interactions with other opiates.
Methadone is detectable in blood tests for approximately 24 hours, whereas urine tests register traces for up to 12 days. Hair follicle testing provides the longest range of detection, in some cases appearing for over three months following dosage.
Intensive inpatient treatment is the industry-preferred standard for methadone detox. This popular treatment option involves clients living at a designated facility for the duration of treatment during which time they receive licensed medical supervision, ongoing medication management and regular psychotherapy. Many inpatient treatment facilities feature an impressive list of benefits and services, including 24/7 staff monitoring and comprehensive aftercare planning.
Medication-assisted treatment (MAT) describes the use of Food and Drug Administration (FDA) approved pharmacological interventions in combination with psychotherapy. Evidence- based therapies frequently include cognitive behavioral therapy (CBT), dialectical behavioral therapy (DBT), motivational interviewing (MI) and trauma-informed therapy. In cases where presenting problems involve the family unity, ongoing family therapy may be recommended and incorporated into the treatment protocol.
Administering methadone in tapering doses during detox is a controversial practice. Due to the highly addictive properties of the drug, proper caution must be taken before resorting to this method. Generally, supplemental medication is used as a foundation to guide safe treatment. According to the National Alliance of Advocates for Buprenorphine Treatment (NAABT) carefully controlled doses of the following evidence-based medications are considered optimal:
Anxiety and depression-related disorders are often precursors to methadone addiction and polysubstance abuse. Post-traumatic stress disorder is also a known precipitating factor that leads many users to self-medicate. These co-existing, or “co-occurring” disorders as they are often called, require professional medical management and psychotherapy to effectively address. Depending upon a client’s specific diagnoses and presenting issues, medications including pregabalin, buspirone, gabapentin and SSRIs are incorporated into the treatment regimen in addition to the aforementioned primary detox medications.
Outpatient treatment is an affordable alternative to inpatient treatment that involves transitional care. In outpatient settings, found in various public and private institutions, clients receive less intensive care and do not live at the facility 24/7. Particularly attractive to clients with demanding personal and professional schedules, outpatient treatment offers many of the same services and benefits as inpatient treatment on a less comprehensive basis.
Methadone is a potent, unpredictable opiate that should never be treated at home. Self-guided detox is statistically proven to lead to unfavorable treatment outcomes, a greater likelihood of future relapse and exposes users to potentially deadly risks. Even casual recreational users benefit from the help of an established treatment protocol and, in more severe cases, medical supervision and medication management are a necessity.
Quitting methadone cold turkey is extremely dangerous and should never be attempted under ANY circumstances. Doing so increases the likelihood of “precipitated withdrawal,” the rapid intensification and acceleration of withdrawal symptoms. As noted above, methadone “dose tapering” is a highly controversial treatment method that subjects the body to the very same substance that created and sustained the addiction. For this reason, carefully controlled doses of other evidence-based medications like Suboxone and Subutex—and only as a short-term treatment intervention—is deemed the safest and most effective approach.
The decision to enter methadone detox and rehabilitation is critical, and individual variables such as location, affordability, insurance coverage, spirituality, and facility reputation must all be considered. The majority of facilities will be able to verify insurance coverage and benefits prior to enrollment which helps ensure a stress-free admission process. In most cases, full or partial coverage is granted. In the unusual event that coverage is denied, additional financial options will be discussed. These include federal grants, private scholarships and other forms of need-based aid.
Empirical evidence suggests that successful completion of inpatient detox is only one necessary component of long-term sobriety. Other factors dictating long-term success rates fluctuate depending upon individual client motivation and strict adherence to a relapse prevention strategy that involves:
Also, remember that methadone overdose is considered a life threatening medical emergency. In the event of overdose— immediately seek professional medical help at a hospital emergency room (ER).
For more about methadone addiction and recovery, check out these related articles:
Western Journal of Medicine. Use of methadone. Jan, 2000.
Journal of Pain. Methadone Safety: A Clinical Practice Guideline from the American Pain Society and College on Problems of Drug Dependence, in Collaboration with the Heart Rhythm Society. April, 2014.
US National Library of Medicine. Pharmacotherapy in the Treatment of Addiction: Methadone. April, 2010.
Journal of Substance Abuse Treatment. Effectiveness of Methadone Maintenance Therapy and Improvement in Quality of Life Following a Decade of Implementation. Oct, 2016.
Post-Graduate Medical Journal. Methadone: applied pharmacology and use as adjunctive treatment in chronic pain. Vol 80, 2018.
Whether you’re researching for yourself or a loved one, Beach House can help. We understand that this is a serious time in your life and that the treatment center you choose matters. We want you to feel comfortable and empowered to make the right decision for yourself, a friend, or a family member. This is why a counselor is waiting and available to answer your questions and help put your mind at ease regarding the next steps. Many of the staff at Beach House have walked in your shoes. If you feel you’re ready or want more information about how to help a loved one, we can help today. You can also learn why we are voted the #1 rehab for addiction treatment in Florida.
We accept most major insurance plans and can verify your benefits quickly and confidentially.
We’re committed to helping you access the care you need, our admissions counselors can guide you through your coverage options and available resources.





"*" indicates required fields