Read the latest and greatest from our team
of incredible specialists.

Beach House Recovery Center » Blog » Oxycodone Detox – Withdrawal Symptoms and Timeline
Oxycodone belongs to a class of narcotic drugs known as opiate analgesics. Frequently prescribed for the management of moderate to severe pain, Oxycodone is classified as a Schedule 8 Substance (highly controlled) by the Drug Enforcement Administration (DEA) in accordance with the Pharmaceutical Benefits Scheme (PBS). This classification involves the highest level of government and law enforcement scrutiny and regulation, requiring doctors to strictly adhere to state laws when prescribing the drug and to receive approval from designated health authorities. The popular brand name “OxyContin”—an extended-release form of the drug used to treat chronic pain—is particularly addicting and has become severely abused in recent years.

 According to the Center for Disease Control (CDC), in 2016, approximately 63,600 people died from opiate overdose, a figure that equates to approximately 115 Americans daily. Tragically, the number of opiate-related deaths was five times higher than it was in 1999, directly or indirectly affecting the lives of millions. Oxycodone interacts with other mind and body altering substances in a dangerously unpredictable way. For example, consuming oxycodone in combination with alcohol increases confusion, impairs breathing, and creates a sense of disorientation. Even more extreme reactions may result from oxycodone’s interaction with certain antidepressants, including delirium, respiratory failure, convulsions, coma or even death.
According to the Center for Disease Control (CDC), in 2016, approximately 63,600 people died from opiate overdose, a figure that equates to approximately 115 Americans daily. Tragically, the number of opiate-related deaths was five times higher than it was in 1999, directly or indirectly affecting the lives of millions. Oxycodone interacts with other mind and body altering substances in a dangerously unpredictable way. For example, consuming oxycodone in combination with alcohol increases confusion, impairs breathing, and creates a sense of disorientation. Even more extreme reactions may result from oxycodone’s interaction with certain antidepressants, including delirium, respiratory failure, convulsions, coma or even death.
Oxycodone works by binding to opiate receptors in the brain and central nervous system. This binding process dulls the sensation of pain, releasing a surge of dopamine in the process. With continued use, the euphoric effect triggered by this surge creates emotional and physiological dependency on the drug, and increasing dosage is required to maintain the same benefit. Unfortunately, oxycodone’s depressant effect on the respiratory system is dangerous—impairing breathing and slowing the heart rate— occasionally turning deadly. Due to the serious and lasting effects of oxycodone addiction, the majority of users need professional, medically managed detox in order to safely recover.
The mental and psychological changes accompanying oxycodone addiction invariably result in withdrawal symptoms—the severity of which depends upon the type, dose and duration of use. Withdrawal symptoms are evaluated upon admission into a detox program, with tools such as the Clinical Opiate Withdrawal Scale (COWS) serving as objective measurements. The scores obtained from the scale then help guide Medication-assisted treatment (MAT) and determine optimal timelines for therapy. Withdrawal symptoms may include, but are not limited to, the following:
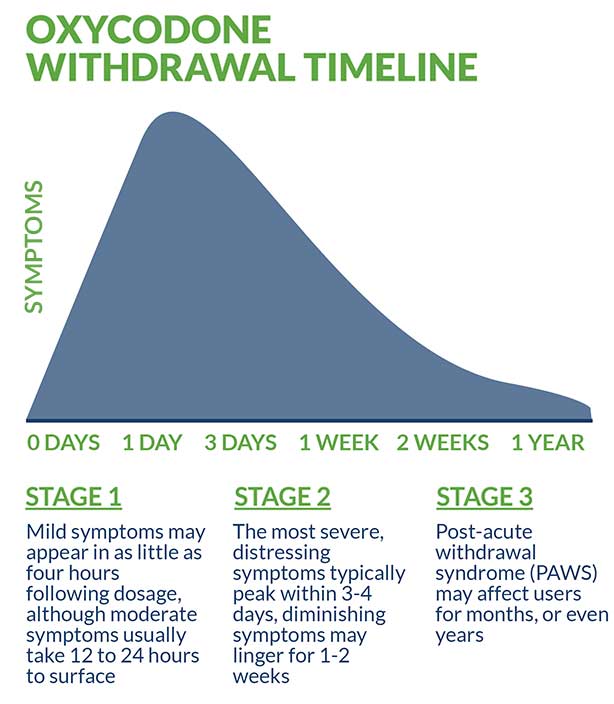
Mild symptoms may appear in as little as four hours following dosage, although moderate symptoms usually take 12 to 24 hours to surface. While the most severe, distressing symptoms typically peak within three to four days, diminishing symptoms may linger for approximately one to two weeks. During this period, medically managed detox is of critical importance as the user is most psychologically fragile and physically vulnerable.
The primary goal of medically managed detox is to prevent the dangerous and potentially deadly onslaught of symptoms, a phenomenon known as “precipitated withdrawal.” Once a user has safely transitioned past the acute withdrawal stage under professional care, they face the long-term effects associated with chronic use. Post-acute withdrawal syndrome (PAWS) may affect users for months, and even years, depending upon the extent of their addiction and variables such as individual biochemistry, age, lifestyle choices and general health.
Oxycodone can be detected via urine samples for up to four days following dosage, whereas blood tests can only detect the drug for 24 hours. Saliva samples are usually detectable from one to four days, with hair testing representing the longest retention period of up to three months.
A multitude of oxycodone treatment options exist; however, intensive inpatient treatment is considered preferential—and for good reason. In addition to the heightened level of medical and clinical supervision by a team of licensed professionals, many facilities provide an impressive range of ancillary services and benefits. Holistic education, creative and expressive arts, alumni networking and ongoing aftercare treatment are all examples of the added value provided by such reputable facilities. Furthermore, client safety and sobriety remain a priority throughout their stay—with the 24/7 staff monitoring and increased security considered optimal.
Medication-assisted treatment (MAT) represents a vital component of oxycodone detox. This approach, which successfully combines pharmacological intervention with behavioral and psychotherapy, provides the foundation for effective treatment. In addition to evidence-based therapies including dialectical behavioral therapy (DBT), cognitive behavioral therapy (CBT), and trauma-informed therapy, the following Food and Drug Administration (FDA) approved medications are frequently incorporated into the treatment regimen:
Oxycodone addiction may occur simultaneously alongside a broad range of anxiety and depression-related disorders and conditions. The presence of “co-occurring disorders” is frequently a precipitating factor involved in opiate addiction—and addiction in general—as is post-traumatic stress disorder (PTSD). Based upon a comprehensive medical and mental health evaluation, a variety of medications may be used to supplement treatment, in addition to the primary medications that form the nucleus of safe, measured oxycodone detox. Pregabalin, buspirone, gabapentin, SSRIs, and a variety of other evidence-based medications are all integral aspects of dual diagnosis management and treatment.
Outpatient treatment is available in a variety of public and private settings (hospitals, clinics, doctors’ offices, rehab centers, etc.) and offers an affordable alternative to inpatient treatment. However, due to the lack of 24/7 monitoring and minimal clinical supervision, it is generally considered less effective. One of the primary advantages associated with outpatient treatment is that it provides greater flexibility—which is desirable for certain clients due to personal and/or professional needs. It also utilizes a less intensive treatment protocol and may be appropriate for clients transitioning from inpatient detox or desiring longer-term sober support.
Self-guided, at-home oxycodone detox is extremely dangerous and never recommended. The physiological and psychological changes that accompany chronic use are capable of triggering a multitude of volatile withdrawal symptoms, none of which can be effectively managed alone. Professional medical assistance and clinical expertise are critical to ensuring optimal treatment outcomes and preventing future relapse. Even in the mildest of cases, self-detox in a home setting leads to less than favorable treatment outcomes and adds to the sense of isolation and disconnectedness frequently responsible for fueling opiate addiction.
A highly controlled, tapered approach to oxycodone detox is generally considered to be the most conservative, safe and effective treatment method. Quitting any medication cold turkey, especially an opiate, gives the body insufficient time to adjust, creating unnecessary risks and complications in the process. This is why—as a recognized industry standard—quitting cold turkey is never recommended or used in reputable treatment facilities.
Ultimately, each client must decide upon the safest and best treatment. Factors affecting this important decision include facility location, affordability and insurance. Insurance is frequently the most important factor, and the majority of facilities will be able to verify insurance coverage and benefits in advance. In the rare event that coverage is not provided, additional options including federal grants, private scholarships and/or flexible payment plans may be available.
Simply completing medically managed detox is not sufficient to ensure long-term recovery success. A key component of long-term abstinence and recovery involves following a multi-pronged approach. Many inpatient facilities can help with strategizing and planning an optimal post-treatment regimen. This should include ongoing medication management, one-on-one and group therapy, life and job skills coaching, regular physical activity, a healthy, nutritious diet, random drug testing and continual sober peer support.
Oxycodone abuse may result in overdose, a life-threatening emergency requiring immediate attention, usually in an emergency room (ER) or intensive care unit (ICU).
For more about oxycodone detox and recovery, check out these related articles:
National Institute on Drug Abuse (NIDA). Opioid Overdose Crises. March, 2018
AMA Journal of Ethics. OxyContin, the FDA, and Drug Control. April, 2014
The Journal of Pain. Comparison of the Risks of Opioid Abuse or Dependence Tepentadol and Oxycodone: Results From a Cohort Study. Oct, 2013
National Center for Injury Prevention and Control. Opioid Overdose Epidemic in the United States. September, 2017.
Journal of the American Academy of Child and Adolescent Psychiatry. Adolescent OxyContin Abuse. February, 2004.
Whether you’re researching for yourself or a loved one, Beach House can help. We understand that this is a serious time in your life and that the treatment center you choose matters. We want you to feel comfortable and empowered to make the right decision for yourself, a friend, or a family member. This is why a counselor is waiting and available to answer your questions and help put your mind at ease regarding the next steps. Many of the staff at Beach House have walked in your shoes. If you feel you’re ready or want more information about how to help a loved one, we can help today. You can also learn why we are voted the #1 rehab for addiction treatment in Florida.
We accept most major insurance plans and can verify your benefits quickly and confidentially.
We’re committed to helping you access the care you need, our admissions counselors can guide you through your coverage options and available resources.





"*" indicates required fields