Marijuana Detox Guide – Withdrawal Symptoms and Timeline
[one-half-first]
The most popular intoxicating drug after alcohol, marijuana has been exalted and vilified, used in ancient religious ceremonies and twenty-first-century medicine, demonized and dismissed…
Records from ancient China show that cannabis, the natural source of marijuana, was known as early as 2727 BCE. Westerners discovered it in the mid-sixteenth century, but used it primarily as a fiber source (hemp) for making rope, paper and cloth. Its first modern medical use was in the 1830s to reduce pain and nausea in cholera patients. In the early twentieth century, Mexican immigrants helped popularize recreational cannabis smoking (and the name “marihuana,” which became “marijuana”) in the United States.
[/one-half-first]
[one-half]
Table of Contents
- Introduction to Marijuana Detox
- Marijuana Withdrawal Symptoms
- Marijuana Withdrawal Timeline
- Inpatient Treatment for Marijuana
- Outpatient Treatment for Marijuana
- Can Marijuana Detox Be Done at Home?
- Tapered vs. Cold Turkey
- Considerations for Marijuana Detox
- Recovery Success and Aftercare Services for Marijuana
[/one-half][clearfix]
The Marijuana Tax Act of 1937 was the first federal law criminalizing cannabis sales: in 1970, the Controlled Substances Act made marijuana a Schedule I drug, meaning it had no recognized medical usefulness. By the 1990s, however, the idea of using it to ease suffering from serious illness was gaining new popularity. Cannabis extracts are now ingredients in some FDA-approved medicines. Since 2012, recreational use of marijuana has also been legalized in several states, though not by the federal government.
Is marijuana ruining your life? Call: (855) 935-2871
MARIJUANA WITHDRAWAL SYMPTOMS
For a long time, marijuana was thought to be non-addictive: the recognized risks were dangerous behavior under the influence, respiratory damage from smoking, possible long-term brain damage and the chance that marijuana use could make it easier to progress to more dangerous drugs. Now, however, medical science recognizes the existence of marijuana use disorder, which affects about four million Americans. (It’s worth noting that marijuana’s potency has significantly increased over the years: the average per-dose amount of key intoxicating ingredient tetrahydrocannabinol was 3.8 percent in 1991, 12.2 percent in 2014.)
When someone with marijuana use disorder attempts to quit the drug, common withdrawal symptoms include:
[one-half-first]
- Insomnia
- Nightmares
- Chronic drowsiness
- Fever, chills or heavy perspiration
- Loss of appetite
- Physical shakiness
- Difficulty concentrating
- Irritability or restlessness
- High anxiety
- Depression
[/one-half-first]
[one-half]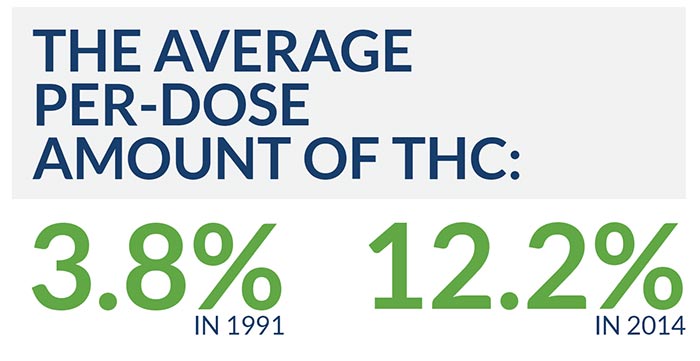
Unlike with many drugs, there is little risk a person will suffer overdose by taking more marijuana when partly detoxed. (Actual cases of marijuana overdose are rare and not tied to any documented fatalities, although symptoms include a high pulse rate that could be dangerous to someone with a weak heart.) The greatest risk of marijuana withdrawal (or overdose) is that anxiety, depression or mental confusion will lead the person undergoing detox to do something physically dangerous.
MARIJUANA WITHDRAWAL TIMELINE
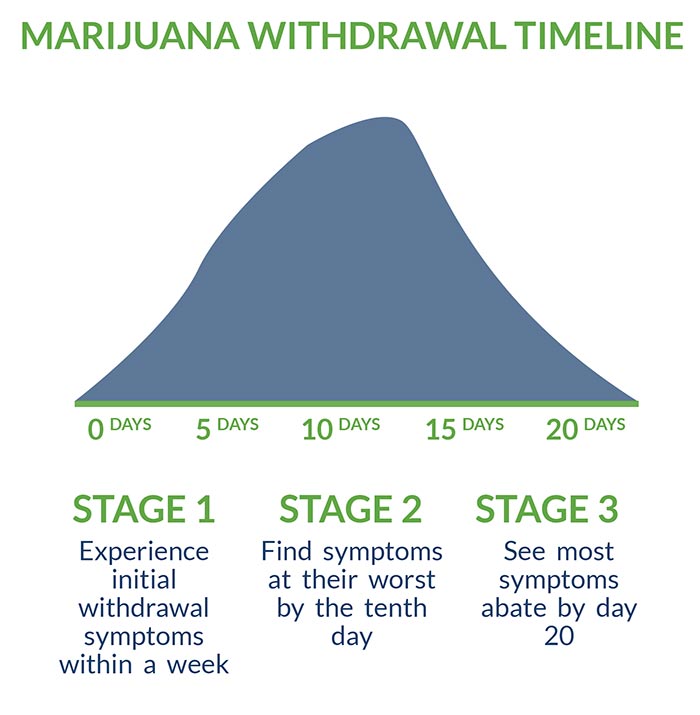
Marijuana has a longer withdrawal period than most addictive drugs. Typically, someone in detox will:
- Experience initial withdrawal symptoms within a week
- Find symptoms at their worst by the tenth day
- See most symptoms abate by day 20
Usually, only people who have used marijuana almost every day for months will be dependent enough to experience symptoms. The more it’s been used, the more unpleasant the withdrawal experience.
INPATIENT TREATMENT FOR MARIJUANA
Someone struggling with that level of dependence often benefits from inpatient treatment (hospitalization for up to three months). Inpatient care is highly recommended if:
- The client client has any co-occurring mental health disorders.
- The has ever seriously considered suicide.
- The client drinks heavily, is taking prescription drugs outside of official medical instructions, or is regularly using illegal drugs besides marijuana. (In any of these cases, an additional addiction disorder may exist that needs inpatient care itself.)
- The client is pregnant. (Almost any drug use or detox can present risks to unborn children: qualified medical advice is essential.)
The advantage of inpatient care is it keeps the client in a supportive environment, protected from relapse temptations and access to marijuana. Since most people with marijuana use disorder struggle with other emotional and life-management issues, those in inpatient treatment also benefit from structured daily schedules and easy access to therapy.
In addition, inpatient treatment allows any needed medications to be prescribed and administered on the spot. While there are no medicines approved specifically to manage cannabis withdrawal, some may be given to treat withdrawal symptoms:
- Sleep aids (e.g., zolpidem or gabapentin) to reduce insomnia
- Anti-anxiety medications (e.g., buspirone) to minimize risks of violent behavior
- Allosteric modulators (e.g., cannabidiol) to reduce cannabis cravings
OUTPATIENT TREATMENT FOR MARIJUANA
Someone whose marijuana use disorder is of short duration, and who has no co-occurring mental-health or substance use disorders, may need only outpatient care (therapy sessions of several hours each, 3–5 times a week). Many people receive inpatient care during the physical-detox period, then transition to outpatient.
A client requesting outpatient care should:
- Be in overall good health
- Use no other drugs
- Still perform well in outside responsibilities
- Live close enough to the treatment center to easily keep all appointments
- Have a solid plan to avoid marijuana relapse
- Have family and friends for encouragement and accountability
As with inpatient treatment, an outpatient client will receive assistance uncovering the reasons he or she became dependent on marijuana, and planning healthier ways to cope. Therapy approaches used to treat marijuana use disorders include:
- Identifying problematic behaviors and replacing unhealthy habits with healthy ones
- Actively rewarding healthy behavior
- Mobilizing a client’s internal resources for rapid change
CAN MARIJUANA DETOX BE DONE AT HOME?
While many people stop marijuana use on their own, this is not recommended for anyone with genuine marijuana use disorder, especially someone who may have other psychiatric illnesses. The risk of dangerous or suicidal behavior is too great.
Staying at a professional detox center during the worst of the physical-withdrawal period is the best decision because:
- A detox center has the facilities to make patients as comfortable as possible.
- Certified detox counselors will prepare patients for dealing with symptoms, and will provide care and reassurance if symptoms become intense.
- Medical staff are well trained in catching and addressing potential complications.
TAPERED VS. COLD TURKEY
With some drug addictions, doctors recommend tapering the substance off slowly (or implementing a “substitution tapering” program that transfers the client to an alternate, safer drug) to spare body and brain the full shock of quitting cold. This is rarely necessary with marijuana, but detox center staff will advise on the best approach for each individual. Most commonly, a client will simply be encouraged to rest, avoid stressful situations and request counseling if needed.
CONSIDERATIONS/HOW TO DECIDE WHAT IS RIGHT FOR YOU
Other factors to consider when choosing a marijuana-detox program include:
- Location (in most cases, it’s preferable the client stay in the same geographical area)
- Special religious or psychological concerns
- The center’s ability to accommodate dietary or special needs
- The center’s reputation
- The center’s experience treating marijuana dependence specifically
- Cost (on the high end, long-term inpatient care can total three or four thousand dollars)
- What health insurance will cover
RECOVERY SUCCESS AND AFTERCARE SERVICES FOR MARIJUANA
With most addiction disorders, the chance of relapsing at least once after initial recovery is 40 to 60 percent. Marijuana use disorder is no exception: the figure may be even higher if previous attempts to quit are factored in.
Relapse needn’t equal a return to full addiction, and there are many resources to both recover from relapse and prevent it in the first place. Organized peer groups, which provide moral support and accountability, improve recovery rates for any toxic habit. A drug detox center can recommend support groups, and may even sponsor groups of its own through an aftercare or alumni program.
Other helpful techniques for staying clean after marijuana detox:
- Continuing in therapy to maintain accountability and develop alternate coping strategies.
- Getting active support from family and friends.
- Avoiding people, places and situations associated with past marijuana use.
- Replacing toxic people, places and situations with healthy ones.
- Pursuing hobbies and social activities to develop natural passions.
- Cultivating an active spiritual life.
- Affirming skills and self-confidence daily.
For related information, see the following articles:
- “Marijuana Detox: 7 Things You Need to Know”
- “The 3 Most Commonly Abused Drugs in the Workplace”
- “How Untreated Drug or Alcohol Addiction Affects Other Health Issues”
Is marijuana ruining your life? Get help now
[expand title=" Sources:" targclass="highlight"]
DEAMuseum.org. “Cannabis: History.” Retrieved from https://www.deamuseum.org/ccp/cannabis/history.html
History.com. “Marijuana.” Retrieved from https://www.history.com/topics/history-of-marijuana
Kathmann, M., K. Flau, A. Redmer, C. Trankle, and E. Schlicker (2006, February). “Cannabidiol Is an Allosteric Modulator at Mu- and Delta-Opioid Receptors.” Naunyn-Schmiedeberg’s Archives of Pharmacology, Vol. 372, No. 5, pp. 354–361. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/16489449
Mason, Barbara J., Rebecca Crean, Vivian Goodell, John M. Light, Susan Quello, Farhad Shadan, Kimberly Buffkins, Mark Kyle, Murali Adusumalli, Adnan Begovic, and Santosh Rao (2012, February 29). “A Proof-of-Concept Randomized Controlled Study of Gabapentin: Effects on Cannabis Use, Withdrawal and Executive Function Deficits in Cannabis-Dependent Adults.” Neuropsychopharmacology, No. 37, pp. 1689–1698. Retrieved from https://www.nature.com/articles/npp201214
National Institute on Drug Abuse (2018, June). “Available Treatments for Marijuana Use Disorders.” Retrieved from https://www.drugabuse.gov/publications/research-reports/marijuana/available-treatments-marijuana-use-disorders
National Institute on Drug Abuse (2018, June). “Can Marijuana Use During and After Pregnancy Harm the Baby?” Retrieved from https://www.drugabuse.gov/publications/research-reports/marijuana/can-marijuana-use-during-pregnancy-harm-baby
National Institute on Drug Abuse (2018, June). “Is Marijuana a Gateway Drug?” Retrieved from https://www.drugabuse.gov/publications/research-reports/marijuana/marijuana-gateway-drug
National Institute on Drug Abuse (2018, June). “Is Marijuana Addictive?” Retrieved from https://www.drugabuse.gov/publications/research-reports/marijuana/marijuana-addictive
National Institute on Drug Abuse (2018, June). “Is Marijuana Safe and Effective as Medicine?” Retrieved from https://www.drugabuse.gov/publications/research-reports/marijuana/marijuana-safe-effective-medicine
National Institute on Drug Abuse (2018, June). “What Are Marijuana Effects?” Retrieved from https://www.drugabuse.gov/publications/research-reports/marijuana/what-are-marijuana-effects
National Institute on Drug Abuse (2018, June). “What Are Marijuana’s Effects on Lung Health?” Retrieved from https://www.drugabuse.gov/publications/research-reports/marijuana/what-are-marijuanas-effects-lung-health
National Institute on Drug Abuse (2018, June). “What Are Marijuana’s Effects on Other Aspects of Physical Health?” Retrieved from https://www.drugabuse.gov/publications/research-reports/marijuana/what-are-marijuana’s-effects-on-other-aspects-of-physical-health%3F
National Institute on Drug Abuse (2018, June). “What Are Marijuana’s Long-Term Effects on the Brain?” Retrieved from https://www.drugabuse.gov/publications/research-reports/marijuana/what-are-marijuanas-long-term-effects-brain
National Institute on Drug Abuse (2018, June). “What Is the Scope of Marijuana Use in the United States?” Retrieved from https://www.drugabuse.gov/publications/research-reports/marijuana/what-scope-marijuana-use-in-united-states
Silverman, Ellie (2017, November 17). “The Truth Behind the ‘First Marijuana Overdose Death’ Headlines.” The Washington Post. Retrieved from https://www.washingtonpost.com/news/to-your-health/wp/2017/11/17/the-truth-behind-the-first-marijuana-overdose-death/?utm_term=.1d8732221804
Thompson, Matt (2013, July 22). “The Mysterious History of ‘Marijuana.’” National Public Radio, Inc. Retrieved from https://www.npr.org/sections/codeswitch/2013/07/14/201981025/the-mysterious-history-of-marijuana
[/expand]