Read the latest and greatest from our team
of incredible specialists.

Beach House Recovery Center » Blog » The Truth About Relapse Rates and Addiction Recovery
Relapse, or the recurrence of drug or alcohol addiction following a period of remission or recovery, is common among those with diagnosed substance use disorders (SUDs). Rates of relapse for drug addiction (40 to 60 percent) generally align with those for other chronic diseases, such as diabetes, asthma, and hypertension, according to a fact sheet from the National Institute on Drug Abuse. However, SUD treatment can help those with a diagnosed addiction reduce their risks of relapse and successfully manage their illness. This article will summarize the latest research on relapse rates and addiction recovery, so that readers and their families can make educated decisions regarding treatment options (such as length and type of treatment and whether to get professional help in the first place).

A number of variables can govern rates of relapse for addiction. For example, participation in a 12-step recovery group like Alcoholics Anonymous (AA) is one evidence-based buffer against relapse. So is the length of participation in AA. One study found that 72 percent of individuals who participated in AA for 27 weeks or more in years two to three were abstinent at 16 years, which is twice as many as those who did not participate.
Nevertheless, two general trends emerge from an overview of the current research regarding SUD treatment and relapse rates: SUD treatment can significantly reduce relapse rates, and relapse rates are highest during the first year of sobriety but decline greatly with each subsequent year of successful abstinence.
With respect to the first trend, there is evidence to show that even a few days of SUD treatment can greatly reduce relapse rates, on the basis of data from the Substance Abuse and Health Administration. A press release from the Partnership for Drug-Free Kids summarized those findings as follows: “Patients who received addiction treatment within 30 days of going through detoxification took 40 percent longer to relapse if they fell off the wagon at all.”
Additional research has confirmed the second trend. A 2007 study published by the National Institutes of Health compared relapse rates during the first year of recovery with those in succeeding years. The conclusion? That whereas only about a third of those in their first year of recovery will remain abstinent, the success rate goes up to more than 50 percent after the one-year mark. For those who have attained five years of sobriety, the projection is dramatically lower: “If you can make it to five years of sobriety, your chance of relapse is less than 15 percent,” an article in Psychology Today concluded, summarizing the results of the same study.
Rates of relapse during alcohol recovery is high for those with alcohol use disorders, and are comparable to rates of relapse for nicotine and heroin. The National Institute on Alcoholism and Alcohol Abuse has cited evidence that 90 percent of alcoholics will experience at least one relapse following treatment, noting that aligns with nicotine and heroin relapse rates.
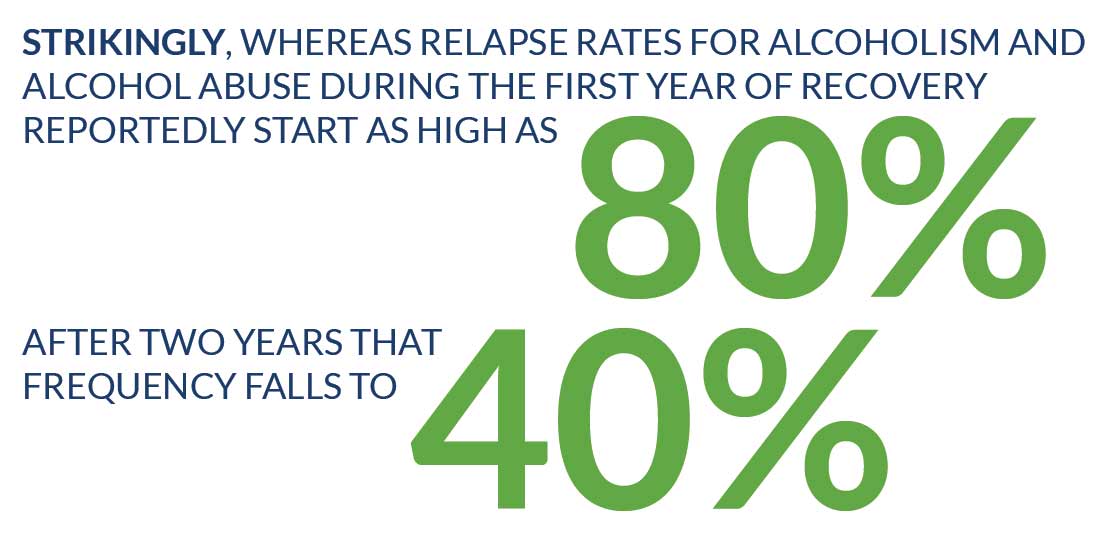 Still, statistics regarding alcohol relapse follow the same general trend of rewarding those who successfully ward off relapse for at least one year. Strikingly, whereas relapse rates for alcoholism and alcohol abuse during the first year of recovery reportedly start as high as 80 percent, after two years that frequency falls to 40 percent.
Still, statistics regarding alcohol relapse follow the same general trend of rewarding those who successfully ward off relapse for at least one year. Strikingly, whereas relapse rates for alcoholism and alcohol abuse during the first year of recovery reportedly start as high as 80 percent, after two years that frequency falls to 40 percent.
What is more, research has found that individuals who seek help for an alcohol use disorder are more likely to be in remission at the third-year mark in recovery than individuals who do not get help for their disease. That was the conclusion of a study in the journal, Addiction. In the study, researchers examined recovery outcomes for those in alcohol treatment and those not in alcohol treatment, by assessing relapse rates at the one-year, three-year, eight-year and 16-year mark. They found those who sought treatment did better.
Relapse rates for the stimulant drugs cocaine and methamphetamine reinforce the same impression that addiction treatment makes a positive difference and can be a significant predictor of recovery. A national study by researchers at the Institute of Behavioral Research at Texas Christian University followed people who had gone through treatment for cocaine addiction over the course of one-year post-rehab. They found that 377 (23.5 percent) of 1,605 individuals were using cocaine weekly within one year of treatment — a significant drop from the 73 percent who were using cocaine weekly before treatment.
The statistics regarding meth relapse rates also favor choosing detox and treatment over detox alone. In one study cited by Reuters, 48 percent of meth users who followed detox with drug rehab was still sober after three months; and 20 percent of those who attended treatment were still abstinent after one year, in contrast to only 7 percent of people who had undergone the only detox or received no treatment.
Like alcohol, opiate addiction exhibits high relapse rates — more than 80 percent among those who receive behavioral treatments alone, the research shows. However, when used in conjunction with behavioral treatments, medication-assisted treatments like Suboxone (buprenorphine) have significantly lowered relapse rates.
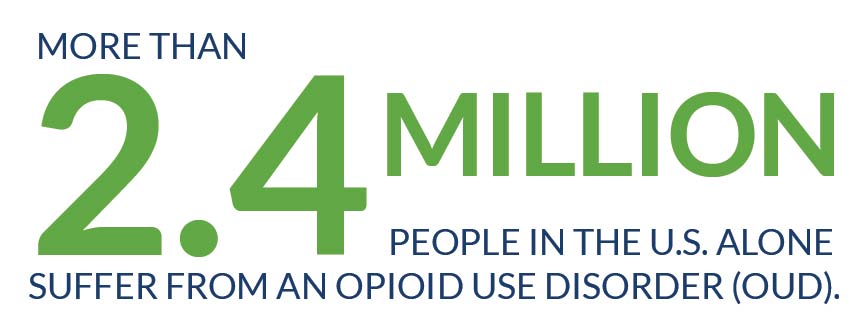 Addiction to opiates is both a serious and growing problem. More than 2.4 million people in the U.S. alone suffer from an opioid use disorder (OUD). The federal government is responding to this health crisis with task forces and a focus on medication-assisted therapies (MAT), as well as funding for the development of effective new pharmacological treatments for opiate addiction. There have been promising results from long-acting buprenorphine subdermal implants that deliver steady-state levels of the opioid agonist, and the Food and Drug Administration (FDA) approved the newest implant, Probuphine® in May 2016. Extended-release naltrexone is now clinically available for those with moderate to severe OUD to help them achieve and maintain abstinence from the opiates and prevent relapse.
Addiction to opiates is both a serious and growing problem. More than 2.4 million people in the U.S. alone suffer from an opioid use disorder (OUD). The federal government is responding to this health crisis with task forces and a focus on medication-assisted therapies (MAT), as well as funding for the development of effective new pharmacological treatments for opiate addiction. There have been promising results from long-acting buprenorphine subdermal implants that deliver steady-state levels of the opioid agonist, and the Food and Drug Administration (FDA) approved the newest implant, Probuphine® in May 2016. Extended-release naltrexone is now clinically available for those with moderate to severe OUD to help them achieve and maintain abstinence from the opiates and prevent relapse.
Every year, more than 300,000 people seek treatment for marijuana addiction, officially termed cannabis use disorder (CUD). Yet, with high relapse rates and no medication to treat CUD currently approved by the Food and Drug Administration (FDA), the push is on to fund and develop effective pharmacotherapy. While a 2013 study in Neuropsychopharmacology points to nabilone offering potential to decrease marijuana withdrawal and relapse to the drug in the laboratory, more recent research published in the journal Psychopharmacology examines the use of zolpidem in combination with nabilone for its apparent ability to reduce marijuana relapse.
What accounts for the high marijuana relapse rates? Factors contributing to marijuana relapse are still relatively unknown. However, in a 2012 study supported by the NIDA, researchers found that daily marijuana smokers who also smoke cigarettes have high rates of marijuana relapse (75 percent in the first study group, 87 percent in the second). Another significant finding was that those who initiated marijuana use later in life were more likely to relapse than those who began daily marijuana smoking at about age 18. Researchers suggest that current cigarette smoking is a “clinical marker for a greater risk of drug relapse.”
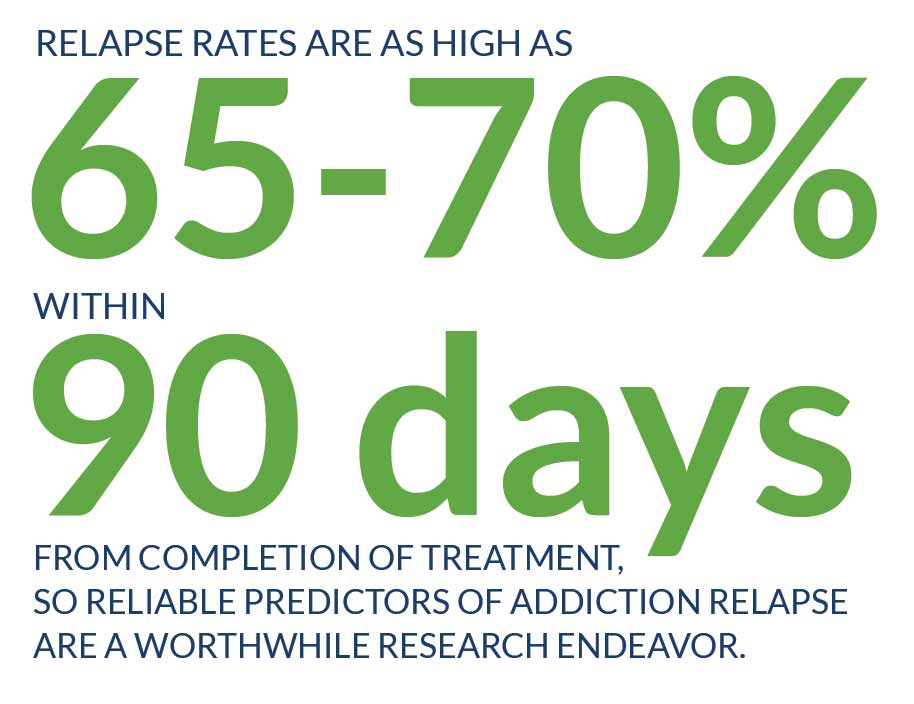 Given that addiction is a chronic, relapsing disease, recent research into the prospect of identifying biological markers of addiction relapse risk is promising. Relapse rates are as high as 65 to 70 percent within 90 days from completion of treatment, so reliable predictors of addiction relapse are a worthwhile research endeavor.
Given that addiction is a chronic, relapsing disease, recent research into the prospect of identifying biological markers of addiction relapse risk is promising. Relapse rates are as high as 65 to 70 percent within 90 days from completion of treatment, so reliable predictors of addiction relapse are a worthwhile research endeavor.
Neural and biological evidence from prospectively designed clinical studies assessing relapse and predicting addiction relapse highlight the following as significant predictors:
The hope is that further research into validating these measures and identifying new measures may lead to the development of an “endopheno-type” for relapse risk that clinicians can use to screen for those most susceptible for relapse. In addition, such markers can be used to gauge treatment effectiveness and to help in the development of new treatments to improve addiction relapse outcomes.
Sources:
Biological Psychiatry. “Predictors of Marijuana Relapse in the Human Laboratory: Robust Impact of Tobacco Cigarette Smoking Status.” Retrieved June 28, 2018.
Current Psychiatry Reports. “New Findings on Biological Factors Predicting Addiction Relapse Vulnerability.” Retrieved June 28, 2018.
Drug Design, Development and Therapy. “New developments in managing opioid addiction: effects of a subdermal buprenorphine implant.” Retrieved June 29, 2018.
Neuropsychopharmacology. “Nabilone decreases marijuana withdrawal and a laboratory measure of marijuana relapse.” Retrieved June 28, 2018.
The American Journal on Addiction. “Antagonists in the medical management of opioid use disorders: History and existing treatment strategies.” Retrieved June 29, 2018.
Psychopharmacology. “Effects of zolpidem alone and in combination with nabilone on cannabis withdrawal and a laboratory model of relapse in cannabis users.” Retrieved June 28, 2018.
Whether you’re researching for yourself or a loved one, Beach House can help. We understand that this is a serious time in your life and that the treatment center you choose matters. We want you to feel comfortable and empowered to make the right decision for yourself, a friend, or a family member. This is why a counselor is waiting and available to answer your questions and help put your mind at ease regarding the next steps. Many of the staff at Beach House have walked in your shoes. If you feel you’re ready or want more information about how to help a loved one, we can help today. You can also learn why we are voted the #1 rehab for addiction treatment in Florida.
We accept most major insurance plans and can verify your benefits quickly and confidentially.
We’re committed to helping you access the care you need, our admissions counselors can guide you through your coverage options and available resources.





"*" indicates required fields