Read the latest and greatest from our team
of incredible specialists.

Beach House Recovery Center » Blog » Suboxone Withdrawal Symptoms & Detox Timeline
Suboxone withdrawal can be physically, mentally, and emotionally challenging, especially if you stop too quickly or without medical support.
In this guide, we explore Suboxone detox symptoms, the withdrawal timeline, and the safest ways to manage the process.

Suboxone is a brand name medication that combines buprenorphine and naloxone to treat opioid use disorder.
Suboxone reduces opioid cravings, minimizes withdrawal symptoms, and lowers the risk of relapse satisfying the brain’s need for opioids in a controlled, less euphoric way.
While Suboxone can be life-changing for many, stopping it too quickly (or without proper medical supervision) can lead to uncomfortable withdrawal symptoms.
Suboxone withdrawal symptoms may resemble heroin withdrawal, though they are generally milder:
Suboxone withdrawal symptoms impact the body and mind, which often interfere with daily responsibilities and increase the risk of relapse if they’re not properly managed.
Physical symptoms may include:
Psychological symptoms may include:
These symptoms often increase in severity for the first 72 hours as the withdrawal progresses.
In more severe cases, withdrawal symptoms may include:
Suboxone Withdrawal Timeline
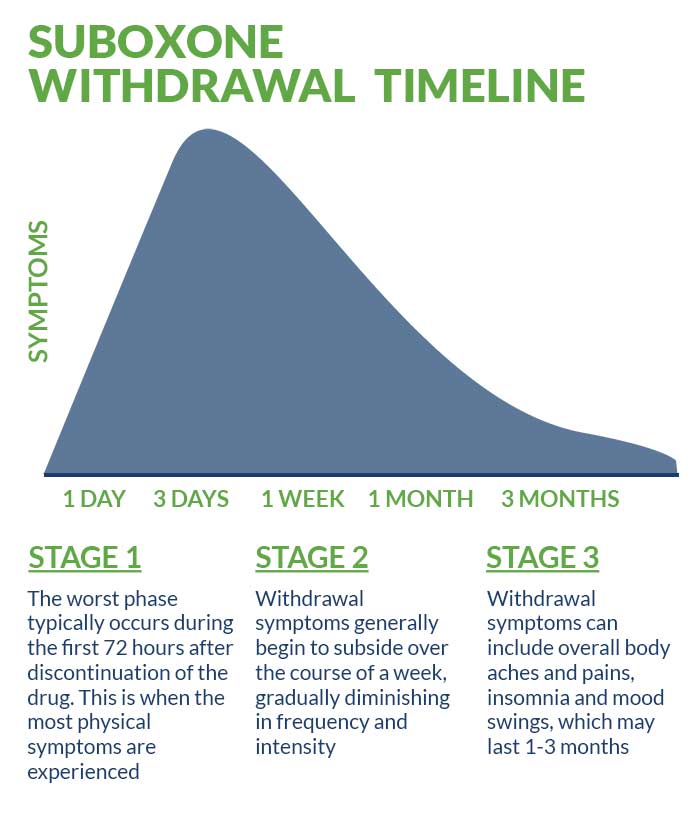
Suboxone’s long half-life (ranging from 36 to 72 hours) means withdrawal typically begins one to three days after the last use, with peak symptoms around day three.
Drug test detection windows:
While acute withdrawal symptoms usually resolve within a week, lingering symptoms like mood swings, sleep issues, and low energy may last for one to three months.
Long-term Suboxone users have a higher risk of depression or an anxiety disorder (that may or may not have been precipitated by withdrawal symptoms) that persists for months.
Stopping “cold turkey” can be dangerous and potentially fatal depending on how long and how much you’ve been using. A gradual taper that’s guided by a medical professional is safer and more effective.
Working with a Beach House Center for Recovery addiction specialist ensures you’ll receive a personalized and medically supported Suboxone detox guide.
Several Suboxone withdrawal medications can help ease symptoms during detox, including:
At Beach House Center for Recovery, we understand that addiction and mental health are often entwined. That’s why we provide the following therapeutic offerings in our treatment programs:
Suboxone detox medications such as clonidine or lofexidine may help:
You can support your medically assisted detox program and help ease discomfort by engaging in these self-care strategies:
If you or your loved one have tried detoxing from Suboxone or other opioids alone without success, are experiencing severe symptoms, or have intense cravings that are putting you at risk for relapse, seeking professional help is critical for your safety and long-term recovery.
Everyone’s detox needs are unique and require a tailored approach. We can help you determine whether an inpatient or outpatient detox program is right for you. All of our detox clients receive high-quality, personalized treatment and daily check ins with our addiction specialists.
We strongly advise against attempting to detox at home. The risk of relapse, overdose, or unmanaged withdrawal is high, especially without knowing how to safely taper.
A medically supervised detox program ensures you’re monitored, supported, and protected every step of the way.
Don’t take the risk. Call Beach House Center for Recovery today and take the first step toward safe, compassionate, and professional Suboxone detox and recovery.
A medically supervised detox program for Suboxone offers:
When undergoing medical detox at Beach House Center for Recovery, you can expect:
Quitting Suboxone suddenly can shock the system, triggering intense withdrawal symptoms and relapse.
Gradual tapering allows your body to slowly adjust to lower doses of Suboxone over time. When done under medical supervision, this method can:
Working closely with your Beach House Center for Recovery addiction specialist ensures the tapering plan is tailored to your needs, ensuring the Suboxone withdrawal process is manageable and safe.
Choosing between inpatient and outpatient detox is a personal decision. It should be based on your
While finances shouldn’t be the only factor, we understand cost is a major concern for many. Financial help may be available through federal, state and local programs. Some treatment facilities also offer sliding scale fees, payment plans, or financing options to reduce out-of-pocket expenses.
The most important question to ask yourself is: “Where will I receive the safest, most supportive care for my recovery?”
Taking time to consider your needs and explore your options can help ensure you select the best path for your needs.
Aftercare is an essential part of recovery and supports long-term sobriety after medical detox.
Our continuing care program helps you:
Here’s how you can maintain sobriety after Suboxone detox at Beach House Center for Recovery:
For more about Suboxone detox and recovery, check out these related articles:
Is Suboxone ruining your life? Get help now
Whether you’re researching for yourself or a loved one, Beach House can help. We understand that this is a serious time in your life and that the treatment center you choose matters. We want you to feel comfortable and empowered to make the right decision for yourself, a friend, or a family member. This is why a counselor is waiting and available to answer your questions and help put your mind at ease regarding the next steps. Many of the staff at Beach House have walked in your shoes. If you feel you’re ready or want more information about how to help a loved one, we can help today. You can also learn why we are voted the #1 rehab for addiction treatment in Florida.
We accept most major insurance plans and can verify your benefits quickly and confidentially.
We’re committed to helping you access the care you need, our admissions counselors can guide you through your coverage options and available resources.





"*" indicates required fields