Klonopin Detox Guide: Withdrawal Symptoms & Timeline
[three-fifths-first]
Klonopin (Clonazepam) belongs to a class of prescription drugs known as benzodiazepines (benzos), which are sedatives commonly used as anti-anxiety and anti-convulsant medications. Klonopin was originally designed by chemist Leo Sternbach in 1955 and later developed and patented in 1964 by Hoffman La Roche Pharmaceuticals in the wake of the meteoric success of other benzos introduced on the market. By the mid 1970’s, the drug was being marketed for the treatment of epileptic seizures, its popularity steadily increasing over the decades. Renowned for its short-term efficacy, Klonopin is rapidly becoming over-abused by teens and young adults— many of whom use the drug illicitly (especially by snorting) to curb anxiety, reduce insomnia and prevent panic attacks.
[/three-fifths-first]
[two-fifths]
TABLE OF CONTENTS
- Introduction to Klonopin Detox
- Klonopin Withdrawal Symptoms
- Klonopin Withdrawal Timeline
- Inpatient Treatment for Klonopin
- Outpatient Treatment for Klonopin
- Can Klonopin Detox Be Done at Home?
- Tapered vs. Cold Turkey
- Considerations for Klonopin Detox
- Recovery Success and Aftercare Services for Klonopin
[/two-fifths][clearfix]

The Center for Disease Control (CDC) further reports that benzo-related overdose deaths spiked dramatically between 2005 and 2013; between the same years, benzo prescriptions rose from 8.1 million to 13.5 million, the Medical Expenditure Panel Survey reported. Klonopin was a major contributor to both of these upward trends.
Is Klonopin ruining your life? Call: (855) 935-2871
KLONOPIN WITHDRAWAL SYMPTOMS
A fast-acting benzodiazepine, Klonopin blocks receptors in the brain that trigger stress and anxiety through the mechanism of increasing the brain neurotransmitter GABA. Once unleashed, this neurotransmitter slows down multiple bodily functions by activating the parasympathetic nervous system. It can take as little as a month to become Klonopin-dependent, with increasing frequency and dosage required to maintain the same short-term effects. Due to the sedating, euphoric “high” induced by the drug, once a user becomes addicted and stops, the brain responds by becoming hyperactive. Klonopin is potent enough that even casual, recreational users may experience significant withdrawal symptoms.
Upon admission into a detox program, a team of trained medical professionals and licensed clinicians help evaluate the severity of Klonopin withdrawal symptoms using a variety of evidence-based tools. These assessments then dictate client-specific treatment goals including when Medication-assisted Treatment (MAT) begins and recommended timelines for therapy. Depending upon whether a user is in late or early stage addiction and how mild or extreme their dosage, the following cluster of Klonopin withdrawal symptoms may occur:
[one-half-first]
- Irritability
- Hallucinations
- Elevated body temperature
- Disorientation
- Insomnia
- Panic Attacks
[/one-half-first][one-half]
- Hand tremors
- Accelerated pulse
- Sweating
- Seizures
- Nausea and/ or vomiting
[/one-half][clearfix]
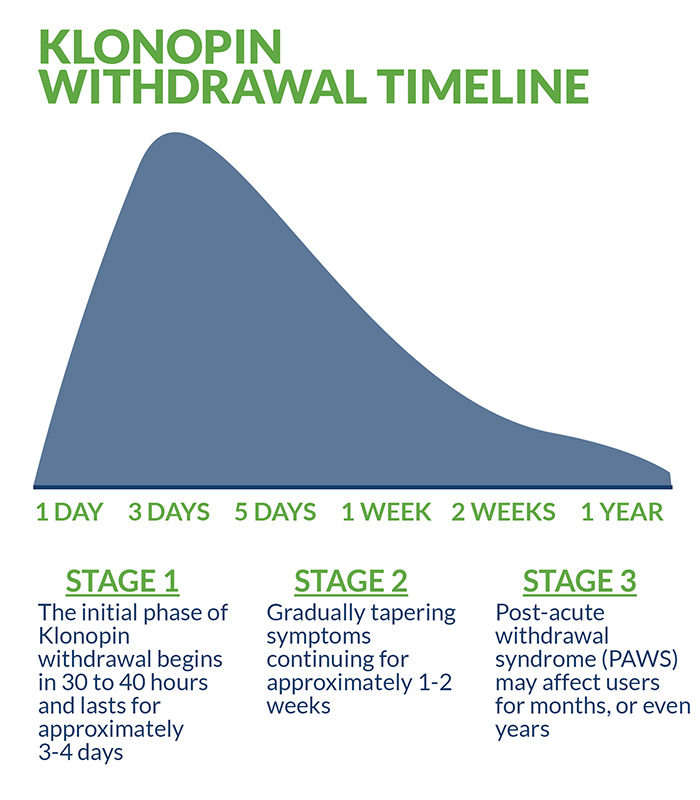
KLONOPIN WITHDRAWAL TIMELINE
The initial phase of Klonopin withdrawal begins once the final dose of the drug exits the bloodstream, a process which generally takes 30 to 40 hours and lasts for approximately three or four days. During this phase, Klonopin withdrawal symptoms are most acute and disorienting in the majority of clients. This phase is followed by the acute withdrawal phase, with gradually tapering symptoms continuing for approximately one to two weeks.
After transitioning through the first two stages of Klonopin withdrawal, users experience a protracted, less intense phase known as post-acute withdrawal syndrome (PAWS). Many factors converge to determine the length of PAWS, such as age, overall mental and physical health, individual biochemistry, and frequency and duration of use. PAWS symptoms may linger for months and even years, presenting the greatest challenge to clients in terms of maintaining their internal motivation toward recovery. Interestingly, emerging research suggests that this protracted phase of withdrawal symptoms is not a result of the Klonopin itself, but of the resurgence of whatever disorder it was originally used to treat.
The approximate half-life of Klonopin is 19 to 60 hours, with average figures ranging from between five and 14 days for the drug to completely leave the system. Benzodiazepines are commonly tested for in pre-employment drug screenings and sobriety tests. Blood, saliva and urine tests can usually detect the drug for up to six days, and hair samples register traces for up to four months.
INPATIENT TREATMENT FOR KLONOPIN
Inpatient treatment for Klonopin is a popular, evidence-based detox option administered under professional medical supervision. The primary advantages of intensive inpatient treatment are the comprehensive range of services, including an intensive level of care, and 24/7 staff monitoring.
Treating benzodiazepine addiction can be particularly difficult— especially since many clients are polysubstance users for whom outpatient treatment is not sufficient. Specialized inpatient detox facilities equipped to handle the full spectrum of benzo treatment offer a significant advantage and follow evidence-based protocols designed to help minimize pain and discomfort during the process. In addition to the heightened level of medical and clinical care, many facilities provide an impressive range of ancillary benefits. Holistic education, creative and expressive arts and comprehensive aftercare services are all examples of the added value provided by such reputable facilities.
Medication-Assisted Treatment
Medication-assisted treatment (MAT) is an integral part of Klonopin detox that combines a tapering schedule of specially selected medicines with behavioral and psychotherapy. Tapering allows the body to gradually return to its normal state while minimizing harsh and potentially deadly backlash effects. After tapering schedules and Food and Drug Administration (FDA)-approved pharmacological interventions are determined by licensed medical professionals, clients receive a variety of evidence-based therapies designed to help treat the emotional and psychological factors associated with Klonopin addiction. Depending upon specific client needs, cognitive behavioral therapy (CBT), dialectical behavioral therapy (DBT), motivational interviewing (MI), and trauma-informed therapy may be included. Additional experiential and expressive therapies are sometimes utilized, as well as ongoing family therapy.
Dual Diagnosis Treatment
Klonopin addiction frequently occurs in tandem with polysubstance abuse and a host of anxiety and depression-related disorders. Post-traumatic stress disorder is another precipitating factor associated with Klonopin addiction, a statistically-proven reason why users try to self-medicate. Dual diagnosis treatment describes the combined treatment of these “co-occurring” disorders—with gabapentin, buspirone, pregabalin, SSRIs and a variety of other evidence-based medications frequently included in the treatment regimen.
OUTPATIENT TREATMENT FOR KLONOPIN
Outpatient facilities provide similar rehabilitation and detox services to those offered by inpatient facilities, only at a less intensive level of care, and are a popular treatment option—especially for clients whose schedules require a greater degree of flexibility. Outpatient treatment is frequently cheaper than inpatient services but considered less effective due to the lack of 24/7 staff monitoring and less intensive level of clinical care. Outpatient programs are excellent intermediary care facilities appropriate for clients who have successfully completed inpatient treatment and desire continued sober support, therapy and 12-step group involvement.
CAN KLONOPIN DETOX BE DONE AT HOME?
Klonopin, like other benzodiazepines, requires a very specific, specialized treatment protocol in order to be effective. Although some users may try to detox at home, doing so is extremely dangerous. Without professional medical supervision, the psychological and physiological effects of the drug can turn deadly. Even in mild to moderate cases, less than optimal treatment outcomes result from self-guided detox creating a greater likelihood of future relapse.
TAPERERED VS COLD TURKEY
Tapering is a widely used detox protocol for the treatment of Klonopin addiction. Tapering subjects the body to carefully controlled, diminishing doses of medication and prevents the dangerous intensification and acceleration of Klonopin withdrawal symptoms. Quitting Klonopin cold turkey results in thousands of visits to emergency rooms annually and should never be attempted under any circumstances. If in doubt about the proper way to address Klonopin addiction, consult a reputable inpatient treatment facility and seek professional medical guidance. The life you might be saving could be your own.
CONSIDERATIONS/HOW TO DECIDE WHAT IS RIGHT FOR YOU
Many factors must be considered before deciding upon the best, most effective treatment plan. The specific substance (or substances, in the case of polysubstance abuse) being treated, program reputability, location and insurance coverage are all key ingredients in making an informed decision. The majority of facilities will be able to verify insurance benefits prior to enrollment, and many clients receive full coverage. In the unusual event that partial, if not total, coverage is denied, additional options such as flexible payment plans and/or other forms of aid may be available.
RECOVERY SUCCESS AND AFTERCARE SERVICES FOR KLONOPIN
Successfully completing an inpatient detox program for Klonopin addiction is only one component of long-term recovery success. An abundance of empirical data highlights the importance of following a comprehensive aftercare program. In addition to maintaining internal motivation, clients benefit most from random drug testing, regular sober peer support, continued one-on-one and/or group therapy, life and jobs skills coaching, healthy diet and regular physical activity, and continuous involvement in 12-step recovery programs. Recovery is a journey fraught with many obstacles and challenges—so choosing a facility that provides adequate aftercare services is vital to ensuring the most favorable treatment outcomes possible.
And remember, Klonopin overdose is considered a life-threatening medical emergency. Immediate treatment, usually in a hospital emergency room (ER) or intensive care unit (ICU) is mandatory.
For more about Klonopin detox and recovery, check out these related articles:
- Snorting Klonopin: Dangers and Side Effects of Snorting this Benzo
- Dangers of Drug Detox at Home and Quitting Cold Turkey
- Common Forms of Prescription Drug Abuse and Their Dangers
- Benzo Addiction: What Makes Benzos So Addictive
Is Klonopin ruining your life? Get help now
[expand title=" Sources:" targclass="highlight"]
Clinical Pharmacology and Neuroscience. The Efficacy and Safety of Clonazepam in Patients with Anxiety Disorder Taking Newer Antidepressants: A Multicenter Naturalistic Study. May, 2016.
Journal of Medicine. A Case Report of Clonazepam Dependence. March, 2016.
The Ochsner Journal. Benzodiazepine Pharmacology and Central Nervous System-Mediated Effects. Summer, 2013.
Journal of Pain and Symptom Management. Clonazepam as an adjuvant analgesic in patients with cancer-related neuropathic pain. December, 2003.
Journal of Medical Case Reports. Clinical considerations in transitioning patients with epilepsy from clonazepam clobazam: a case series. December, 2014.
[/expand]