 The Journal of the American Medical Association
The Journal of the American Medical Association (JAMA) reports that in 2016 approximately half of all opiate-related deaths involved fentanyl—with fentanyl’s role in overdose deaths increasing from 14.3 percent in 2010, to 46 percent in 2016. Fentanyl’s potency is considered approximately 100 times greater than morphine and 50 times greater than heroin. Fentanyl penetrates the brain—where it is quickly absorbed but slowly eliminated. This slow elimination impairs breathing and slows heart rates, frequently resulting in fatalities. Fentanyl is, without question, a killer.
FENTANYL WITHDRAWAL SYMPTOMS
Fentanyl, like other opiates, binds to opiate receptors in the brain and central nervous system. These receptors control the user’s perception of pain and emotion by artificially elevating dopamine levels. The resulting euphoria this creates is highly desirable. The effects, however, wear off quickly and increasing doses are required to maintain the same “high.” Over time, usage creates tolerance to the drug and interferes with the healthy functioning of multiple psychological and physiological processes.
Once a user suffers from full-blown fentanyl addiction, withdrawal symptoms are certain to occur. Because of fentanyl’s unusual potency, chronic users may experience intensified withdrawal symptoms. Withdrawal symptoms are evaluated upon admission into a detox program using reliable tools such as the Clinical Opiate Withdrawal Scale (COWS). Once objective scores are obtained, a team of licensed medical professionals and qualified clinicians work together to implement Medication-assisted treatment (MAT) and design a client-specific plan of action. The following symptoms may be expected and vary widely depending upon what stage of withdrawal a user is experiencing:
- Irritability
- Restlessness
- Headache
- Sweating
- Muscle pain and cramping
- Nausea
- Vomiting
- Insomnia
- Tremors
- Disorientation
- Loss of Appetite
- Diarrhea
FENTANYL WITHDRAWAL TIMELINE
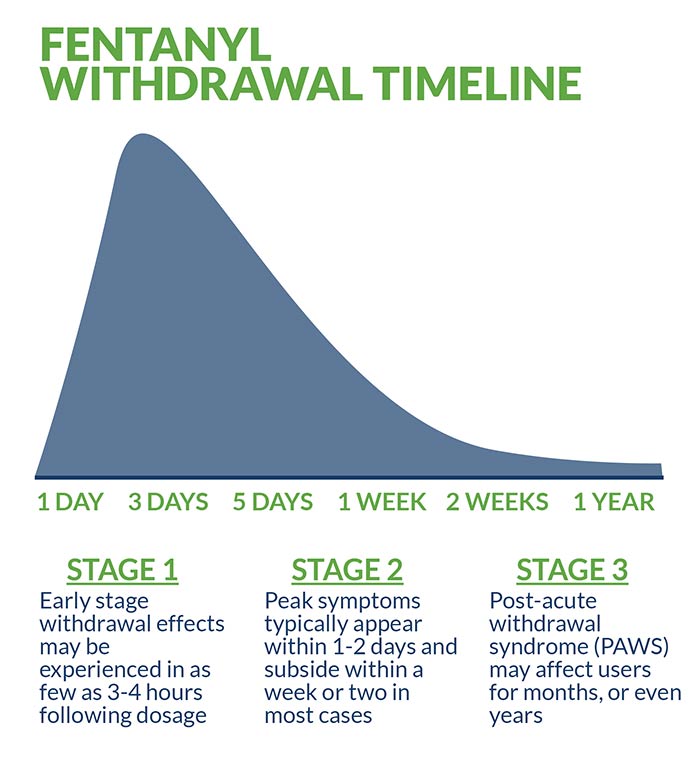
Fentanyl withdrawal timelines can be particularly difficult to establish due to the multiple illicit forms in which the drug appears. These non-pharmaceutical varieties—laced with illicit drugs such as heroin— inject the withdrawal process with an element of uncertainty. In general, early stage withdrawal effects may be experienced in as few as three or four hours following dosage. Peak symptoms typically appear within 1-2 days and subside within a week or two in most cases.
After enduring the initial acute withdrawal stage, a client in early recovery from fentanyl transitions to a longer, less intense phase known as post-acute withdrawal symptom (PAWS). Depending upon the intensity and duration of their fentanyl addiction, PAWS may affect users for months, or even years. In rare instances, permanent damage is sustained as a result of the potent and unpredictable drug’s interaction with individual biochemistry. One of the primary goals of fentanyl detox is to minimize or prevent “precipitated withdrawal,” the rapid and potentially dangerous acceleration of withdrawal symptoms.
Fentanyl may be undetectable by urine under certain circumstances, but in designated tests it may appear for up to 24 hours. Saliva tests generally detect the drug for a period of 1-3 days (less than other opiates). Fentanyl is relatively short-lived in the blood stream, with a maximum duration of approximately 12 hours. Hair samples provide the most accurate long-term result, with traces appearing for up to 90 days following dosage.
INPATIENT TREATMENT FOR FENTANYL
Due to fentanyl’s extreme potency and associated dangers, inpatient treatment is strongly recommended. Only intensive inpatient treatment provides the 24/7 monitoring and increased security necessary to help stabilize clients recovering from the addictive and debilitating effects of the drug. Inpatient treatment includes ongoing assessment and evaluation by a team of licensed medical professionals and qualified clinicians—with many reputable facilities providing additional holistic services and ancillary benefits. This comprehensive, client-focused quality of care is why inpatient treatment is generally considered the industry “gold standard.”
Medication-Assisted Treatment
Medication-assisted treatment (MAT) provides the foundation for fentanyl detox. This popular protocol combines behavioral and psychotherapy in tandem with Food and Drug Administration-approved pharmacological interventions for maximum benefit. Dialectical behavioral therapy (DBT),
motivational interviewing (MI), trauma-informed therapy, family therapy, and cognitive behavioral therapy (CBT) are among the many evidence-based therapies frequently included in the scope of Medication-assisted treatment (MAT)—along with the following medications:
- Vivitrol targets the same brain receptors as fentanyl while blocking the undesirable effects.
- Clonidine helps reduce some of the harsher physical and mental effects of detox.
- Suboxone, which contains the active ingredients buprenorphine and naloxone, produces a similar but less potent effect when compared to fentanyl, thereby relieving withdrawal symptoms and diminishing cravings without the dangers of overdose. The gold standard MAT for fentanyl abuse and addiction is the short-term administration of Suboxone combined with behavioral therapies.
- Subutex (which contains only buprenorphine) produces a similar but less potent effect when compared to oxycodone. Like Suboxone, Subutex can relieve fentanyl withdrawal symptoms and diminish cravings.
- Methadone remains a MAT that some rehab providers and so-called methadone maintenance clinics use for opiate use disorders like fentanyl. Methadone for treating fentanyl dependency is controversial, however, because methadone itself is associated with high rates of dependency and can require supervised detox.
Dual Diagnosis Treatment
Frequently, anxiety and depression-related disorders are the driving force behind fentanyl addiction—in addition to post-traumatic stress disorder (PTSD). Untreated, these disorders create an ongoing psychological and physiological imbalance that users seek to self-medicate—which ultimately leads to addiction.
The treatment of “co-occurring” disorders is a key ingredient in successful detox for many clients, especially those for whom polysubstance abuse and unresolved trauma play a precipitating role. Supplemental medications such as gabapentin, pregabalin, buspirone and SSRIs may be included in the treatment protocol depending upon specific client needs, and are prescribed only after careful evaluation and assessment by a team of licensed medical professionals.
OUTPATIENT TREATMENT FOR FENTANYL
Outpatient treatment offers many of the same services and benefits as inpatient treatment, but without the intensive level of clinical care, 24/7 monitoring and additional security. Typically cheaper than inpatient treatment and less effective, it offers the singular advantage of greater flexibility for certain clients based upon their personal and/or professional schedules. It is also useful for those clients successfully transitioning from more intensive levels of care.
CAN FENTANYL DETOX BE DONE AT HOME?
Fentanyl is a killer—and home detox is never recommended under any circumstances. Not only does self-guided detox lead to unfavorable treatment outcomes, it multiplies the dangers associated with this potent, unpredictable drug. Professional medical supervision and management combined with focused clinical care are required in order to achieve optimal treatment outcomes.
TAPERED VS COLD TURKEY
The safest, most effective fentanyl detox involves administering controlled doses of medication on a tapered basis. Considering the deadly potency of fentanyl and the unknown risks associated with non-pharmaceutical varieties of the drug, quitting cold turkey is never recommended. Professional medical assistance is a critical aspect of treatment, with dose “tapering” allowing the body a sufficient adjustment period while gradually eliminating the drug.
To taper off fentanyl, a person may be first switched to another opiate like Suboxone, after which time the amount of Suboxone is gradually reduced daily, coterminous with behavioral therapies that treat the roots of fentanyl abuse.
CONSIDERATIONS/HOW TO DECIDE WHAT IS RIGHT FOR YOU
Deciding upon what treatment to choose depends upon a variety of factors—the most important of which are affordability, location and insurance. In the majority of cases, insurance coverage and benefits are verified prior to admission, and clients receive partial (if not total) coverage for detox services. If, for some reason, a satisfactory level of insurance compensation is not achieved, additional options such as private scholarships, federal grants and other forms of assistance may be available.
RECOVERY SUCCESS AND AFTERCARE SERVICES FOR FENTANYL
Long-term recovery outcomes depend largely upon individual client motivation and strict adherence to working a multifaceted recovery program. It is imperative for clients to follow a comprehensive aftercare plan that includes one-on-one and/or group therapy (not limited to NA or 12-Step), ongoing medication management and random drug testing. Additionally, regular physical activity, life and job skills coaching, a healthy diet, and regular sober support add an extra, evidence-based benefit.
Remember, fentanyl overdose may result in a life-threatening medical emergency. Immediate treatment in a hospital emergency room (ER) room or intensive care unit (ICU) is required.
For more about fentanyl detox and recovery, check out these related articles:
May, 2017.
AMA Journal of Ethics.
Opioids for Nonmalignant Chronic Pain. March, 2015.
Journal of American Physicians and Surgeons. Estimating the Actual Death Rate Caused by Prescription Opioid Medication and Illicit Fentanyl. Vol. 13. Spring, 2018.
National Institute of Drug Abuse (NIDA) What is Fentanyl? June, 2016.
Association of American Physicians and Surgeons. Opioid Overdose Crisis is From Illicit Fentanyl. Mar, 2018.


 The Journal of the American Medical Association (JAMA) reports that in 2016 approximately half of all opiate-related deaths involved fentanyl—with fentanyl’s role in overdose deaths increasing from 14.3 percent in 2010, to 46 percent in 2016. Fentanyl’s potency is considered approximately 100 times greater than morphine and 50 times greater than heroin. Fentanyl penetrates the brain—where it is quickly absorbed but slowly eliminated. This slow elimination impairs breathing and slows heart rates, frequently resulting in fatalities. Fentanyl is, without question, a killer.
The Journal of the American Medical Association (JAMA) reports that in 2016 approximately half of all opiate-related deaths involved fentanyl—with fentanyl’s role in overdose deaths increasing from 14.3 percent in 2010, to 46 percent in 2016. Fentanyl’s potency is considered approximately 100 times greater than morphine and 50 times greater than heroin. Fentanyl penetrates the brain—where it is quickly absorbed but slowly eliminated. This slow elimination impairs breathing and slows heart rates, frequently resulting in fatalities. Fentanyl is, without question, a killer.
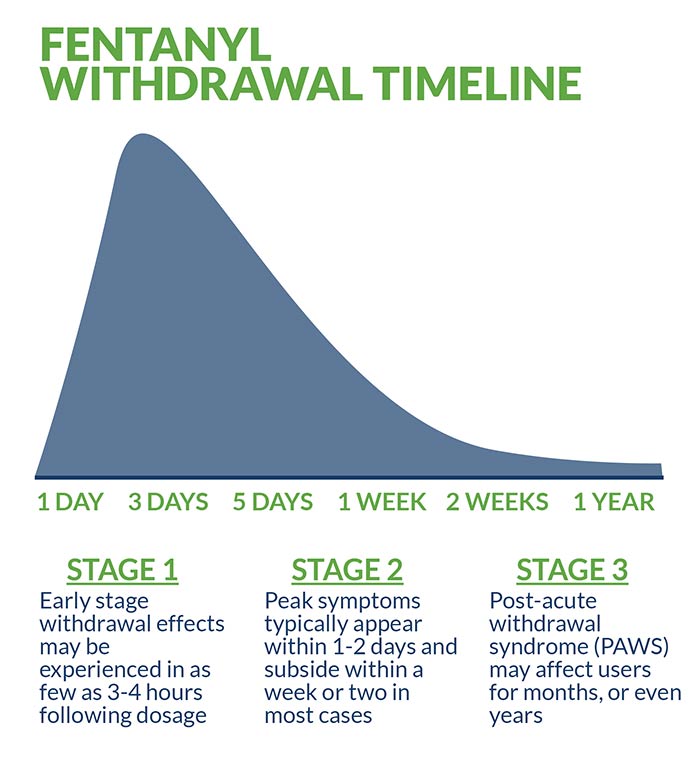 Fentanyl withdrawal timelines can be particularly difficult to establish due to the multiple illicit forms in which the drug appears. These non-pharmaceutical varieties—laced with illicit drugs such as heroin— inject the withdrawal process with an element of uncertainty. In general, early stage withdrawal effects may be experienced in as few as three or four hours following dosage. Peak symptoms typically appear within 1-2 days and subside within a week or two in most cases.
After enduring the initial acute withdrawal stage, a client in early recovery from fentanyl transitions to a longer, less intense phase known as post-acute withdrawal symptom (PAWS). Depending upon the intensity and duration of their fentanyl addiction, PAWS may affect users for months, or even years. In rare instances, permanent damage is sustained as a result of the potent and unpredictable drug’s interaction with individual biochemistry. One of the primary goals of fentanyl detox is to minimize or prevent “precipitated withdrawal,” the rapid and potentially dangerous acceleration of withdrawal symptoms.
Fentanyl may be undetectable by urine under certain circumstances, but in designated tests it may appear for up to 24 hours. Saliva tests generally detect the drug for a period of 1-3 days (less than other opiates). Fentanyl is relatively short-lived in the blood stream, with a maximum duration of approximately 12 hours. Hair samples provide the most accurate long-term result, with traces appearing for up to 90 days following dosage.
Fentanyl withdrawal timelines can be particularly difficult to establish due to the multiple illicit forms in which the drug appears. These non-pharmaceutical varieties—laced with illicit drugs such as heroin— inject the withdrawal process with an element of uncertainty. In general, early stage withdrawal effects may be experienced in as few as three or four hours following dosage. Peak symptoms typically appear within 1-2 days and subside within a week or two in most cases.
After enduring the initial acute withdrawal stage, a client in early recovery from fentanyl transitions to a longer, less intense phase known as post-acute withdrawal symptom (PAWS). Depending upon the intensity and duration of their fentanyl addiction, PAWS may affect users for months, or even years. In rare instances, permanent damage is sustained as a result of the potent and unpredictable drug’s interaction with individual biochemistry. One of the primary goals of fentanyl detox is to minimize or prevent “precipitated withdrawal,” the rapid and potentially dangerous acceleration of withdrawal symptoms.
Fentanyl may be undetectable by urine under certain circumstances, but in designated tests it may appear for up to 24 hours. Saliva tests generally detect the drug for a period of 1-3 days (less than other opiates). Fentanyl is relatively short-lived in the blood stream, with a maximum duration of approximately 12 hours. Hair samples provide the most accurate long-term result, with traces appearing for up to 90 days following dosage.




