According to the 2014 National Survey on Drug Use and Health, over 50 percent of prescription painkillers were illicitly obtained—usually through a friend or relative—with only 22 percent being legitimately prescribed by a doctor.
In 2017, a staggering 33 million Americans were estimated to use codeine, making it one of the most over-prescribed, recreationally abused opiates on the market. Codeine undeniably feeds
America’s opiate epidemic, costing taxpayers billions of dollars annually in lost wages, mass incarcerations and skyrocketing insurance rates.
CODEINE WITHDRAWAL SYMPTOMS
Codeine, like other opiates, produces a wide range of psychological and physiological withdrawal symptoms when used regularly. Although generally not life-threatening, these withdrawal symptoms can rapidly intensify— resulting in serious and potentially deadly complications. For the majority of chronic users, treatment at an inpatient detox facility is imperative to ensure optimal outcomes and provide maximum stabilization during early recovery. Factors including length of addiction, frequency of use and intensity of dosage all combine to determine the severity and extent of withdrawal symptoms.
Upon entry into a medically supervised detox program, clients are evaluated using a variety of clinical tools and measurements. One such tool, the Clinical Opiate Withdrawal Scale (COWS), assesses the severity of symptoms based upon quantifiable scores. In addition to information gained though a battery of other medical and psychiatric assessments, these scores provide the basis for establishing medication-assisted treatment (MAT) timelines and determining optimal therapies. Depending upon whether a client is in early or late stage withdrawal, they may experience the following symptoms:
- Headaches
- Insomnia
- Fever
- Muscle Pain
- Sweating
- Fatigue
- Digestive upset
- Nausea and Vomiting
- Dehydration
- Disorientation
- Mood Swings
CODEINE WITHDRAWAL TIMELINE
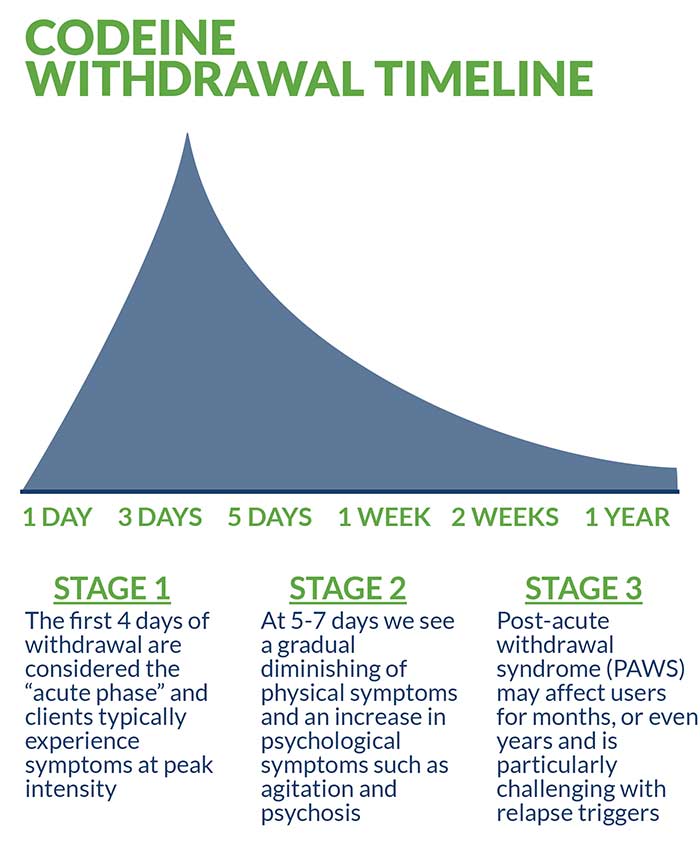
The first four days of withdrawal are considered the “acute phase” and clients typically experience symptoms at peak intensity. After successfully transitioning out of the acute phase, clients enter a moderate phase (five to seven days) that includes the gradual diminishing of certain physical symptoms in conjunction with an increase in psychological symptoms such as agitation and psychosis.
Although codeine withdrawal symptoms subside within one to two weeks for the majority of clients, lingering symptoms may be experienced for months, or even years. This protracted phase is known as post-acute withdrawal syndrome (PAWS) and is particularly challenging in the face of social and environmental relapse triggers. Regardless of which stage of codeine withdrawal a client is in, the primary objective of medically supervised detox remains to prevent “precipitated withdrawal,” the rapid acceleration and intensification of symptoms.
Codeine has a relatively short half-life of approximately three to four hours, while the primary effects generally leave the body within 16 hours. Codeine is detectable in saliva samples for up to four days and urine for over a week, whereas blood tests can only detect the opiate for up to 16 hours. Hair samples provide the longest range of detection, with traces appearing for up to three months.
INPATIENT TREATMENT FOR CODEINE
Inpatient treatment is a popular, empirically proven method of addiction treatment in which clients live at a designated facility, usually for a month but sometimes longer. During their stay, clients receive ongoing medical management and intensive clinical supervision. In addition to the heightened security and 24/7 staff monitoring, clients also enjoy a strong sober support network and increased camaraderie. Beyond these attractive, evidence-based benefits, many state-of-the-art facilities offer amenities such as yoga, meditation, group outings and recreational activities, alumni networking, and ongoing aftercare services.
Medication-Assisted Treatment
Medication-assisted treatment is an integral part of inpatient detox that utilizes Food and Drug Administration (FDA) approved pharmacological interventions in combination with psychotherapy. Depending upon the client-specific treatment plan, a robust variety of therapies such as dialectical behavioral therapy (DBT), cognitive behavioral therapy (CBT), motivational interviewing (MI), and trauma-informed therapy may be included. These therapies help treat the underlying emotional and psychological factors associated with codeine addiction, while the following medications are commonly utilized:
- Suboxone provides a controlled, long-lasting dose of opiates without producing the same euphoric high as methadone.
- Subutex produces a similar but less potent effect when compared to methadone which helps in reducing withdrawal symptoms and diminishing cravings.
Dual-Diagnosis Treatment
A critical aspect of medically supervised detox is the treatment of “co-occurring” disorders—the depression and anxiety-related conditions that precipitate codeine addiction. For example, bipolar disorder, generalized anxiety disorder (GAD), clinical depression, post-traumatic stress disorder (PTSD), and borderline personality disorder (BPD) are all frequently associated with codeine addiction. Depending upon a client’s primary diagnosis and pharmacological intervention, medications such as buspirone, pregabalin, gabapentin and SSRIs may also be used to help achieve maximum benefit.
OUTPATIENT TREATMENT FOR CODEINE
Outpatient treatment is another popular option that involves a more transitory level of care. In outpatient facilities, clients do not live on the premise; however, similar treatment methods are employed. Outpatient treatment is cheaper than inpatient treatment due to the less intensive nature of rehabilitation services— but also less effective. Certain clients require outpatient treatment in light of their demanding personal and/or professional schedules. Outpatient treatment is also optimal for clients successfully transitioning from inpatient detox.
CAN CODEINE DETOX BE DONE AT HOME?
Because over-the-counter varieties of codeine are known as “less potent” than other opiates, users may sometimes resort to self-guided care in the convenience of their own home. This practice is never recommended under any circumstance because it invariably results in sub-optimal treatment outcomes. Although it can be easy to underestimate the damage codeine addiction inflicts upon the body and mind, the proper approach to safely recovering from its effects always includes professional medical supervision and licensed clinical care.
TAPERED VS COLD TURKEY
Tapering is a controversial detox protocol that involves administering carefully controlled doses of codeine while the client phases out of active use. Tapering injects the body with the very same substance that created the addiction in the first place and, in the opinion of many experts, entails unnecessary complications and risks. By the same token, quitting codeine (or any opiate) cold turkey is never recommended, and in extreme cases may even turn deadly. For this reason, supplemental medications like Suboxone and Subutex form a safe, effective basis for codeine treatment without resorting to either extreme.
CONSIDERATIONS/HOW TO DECIDE WHAT IS RIGHT FOR YOU
There is no one-size-fits-all treatment option that works for everyone. Ultimately, each client must decide what is optimal based upon their individual needs and long-term goals. Facility location, affordability, reputation and insurance coverage are all major factors to be considered before arriving at an informed decision. Spirituality and faith also play a significant role in determining treatment for many clients, especially since holistic and faith-based options now exist.
Although insurance is the single greatest concern for the majority of clients, most facilities will be able to verify coverage and benefits prior to enrollment. In the rare event that coverage is denied, admissions staff will discuss a range of additional financial options including federal grants, private scholarships and /or other forms of aid.
RECOVERY SUCCESS AND AFTERCARE SERVICES FOR CODEINE
Following successful completion of inpatient detox, clients are faced with the long-term challenge of maintaining sobriety and avoiding triggers that lead to relapse. While individual motivation and family support help dictate treatment outcomes, an abundance of evidence shows that the following relapse prevention strategy yields the best results:
- 12-step and NA involvement
- Sponsorship
- Continuing medication management
- Random drug testing
- Life and jobs skills coaching
- Sober peer support
- Healthy diet and physical activity
- One-on-one and/or group therapy
In many cases, reputable inpatient treatment facilities provide aftercare services, with some planning a specific regimen in cooperation with the client during their stay. This helps ensure post-treatment success.
For more about codeine addiction and detox, check out these related articles:
Sources:
The American Academy of Pediatrics Clinical Report. Codeine: Time to Say “No.” September, 2016.
Pharmaceutical Methods. Recent Updates on Codeine. Jan, 2011.
The Australian Prescriber. Cautions with codeine. Oct, 2011.
New England Journal of Medicine. New Evidence About an Old Drug—Risk with Codeine After Adenotonscillectomy. Jun, 2013.
JMIR Public Health and Surveillance. Representations of Codeine Misuse on Instagram: Content Analysis. Jan, 2018.
National Institute on Drug Abuse (NIDA). Recent Opiate Overdose Statistics. March, 201


 According to the 2014 National Survey on Drug Use and Health, over 50 percent of prescription painkillers were illicitly obtained—usually through a friend or relative—with only 22 percent being legitimately prescribed by a doctor. In 2017, a staggering 33 million Americans were estimated to use codeine, making it one of the most over-prescribed, recreationally abused opiates on the market. Codeine undeniably feeds America’s opiate epidemic, costing taxpayers billions of dollars annually in lost wages, mass incarcerations and skyrocketing insurance rates.
According to the 2014 National Survey on Drug Use and Health, over 50 percent of prescription painkillers were illicitly obtained—usually through a friend or relative—with only 22 percent being legitimately prescribed by a doctor. In 2017, a staggering 33 million Americans were estimated to use codeine, making it one of the most over-prescribed, recreationally abused opiates on the market. Codeine undeniably feeds America’s opiate epidemic, costing taxpayers billions of dollars annually in lost wages, mass incarcerations and skyrocketing insurance rates.
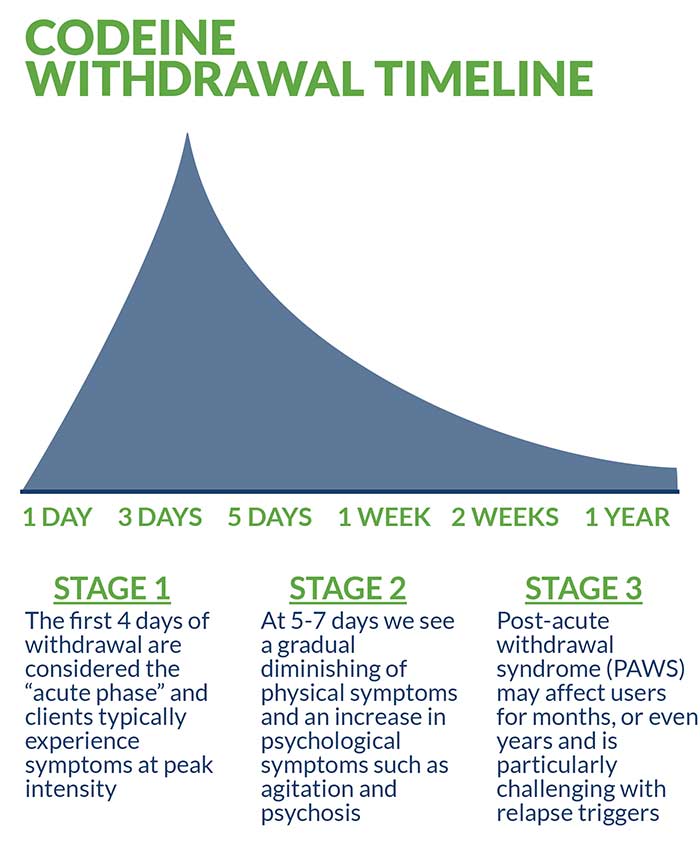 The first four days of withdrawal are considered the “acute phase” and clients typically experience symptoms at peak intensity. After successfully transitioning out of the acute phase, clients enter a moderate phase (five to seven days) that includes the gradual diminishing of certain physical symptoms in conjunction with an increase in psychological symptoms such as agitation and psychosis.
Although codeine withdrawal symptoms subside within one to two weeks for the majority of clients, lingering symptoms may be experienced for months, or even years. This protracted phase is known as post-acute withdrawal syndrome (PAWS) and is particularly challenging in the face of social and environmental relapse triggers. Regardless of which stage of codeine withdrawal a client is in, the primary objective of medically supervised detox remains to prevent “precipitated withdrawal,” the rapid acceleration and intensification of symptoms.
Codeine has a relatively short half-life of approximately three to four hours, while the primary effects generally leave the body within 16 hours. Codeine is detectable in saliva samples for up to four days and urine for over a week, whereas blood tests can only detect the opiate for up to 16 hours. Hair samples provide the longest range of detection, with traces appearing for up to three months.
The first four days of withdrawal are considered the “acute phase” and clients typically experience symptoms at peak intensity. After successfully transitioning out of the acute phase, clients enter a moderate phase (five to seven days) that includes the gradual diminishing of certain physical symptoms in conjunction with an increase in psychological symptoms such as agitation and psychosis.
Although codeine withdrawal symptoms subside within one to two weeks for the majority of clients, lingering symptoms may be experienced for months, or even years. This protracted phase is known as post-acute withdrawal syndrome (PAWS) and is particularly challenging in the face of social and environmental relapse triggers. Regardless of which stage of codeine withdrawal a client is in, the primary objective of medically supervised detox remains to prevent “precipitated withdrawal,” the rapid acceleration and intensification of symptoms.
Codeine has a relatively short half-life of approximately three to four hours, while the primary effects generally leave the body within 16 hours. Codeine is detectable in saliva samples for up to four days and urine for over a week, whereas blood tests can only detect the opiate for up to 16 hours. Hair samples provide the longest range of detection, with traces appearing for up to three months.




