Better detox completion rates
Research has suggested that clients who undergo drug or alcohol detox in inpatient rehab are more likely to successfully complete detox. A 1989 study published in the New England Journal of Medicine compared the effectiveness, safety and costs of outpatient and inpatient detox from alcohol, and found that “significantly more inpatients (95 percent) than outpatients (72 percent) completed detoxification.” In this particular study, the outpatient clients received once-daily medical and psychiatric evaluations and treatment, while the inpatient patients received comprehensive, 24/7 psychiatric and medical evaluation and treatment, followed by follow-up therapies.
One explanation for the better detox completion rates may be the fact that research cited by the American Society of Addiction Medicine has shown that inpatient detox is superior to outpatient detox.
And better detox completion rates accord with better recovery outcomes. A publication by Harvard researchers helps to illustrate how this is so in cases of opiate addiction, for example. Opiate withdrawal symptoms can be uncomfortable, the researchers explained—the implication being that those who undertake opiate withdrawal without medical supervision put themselves at higher risk of relapsing. The researchers went on to explain, moreover, that even a supervised withdrawal is “not a solution” in effectively treating opiate addiction because most opiate addicts will return to using without timely follow- up treatment. And inpatient rehab can ensure that integrated follow-up care following detox.
The immediate transition from detox to inpatient services
A related benefit, then, is the fact that inpatient rehab typically allows clients to transition more quickly from detox to follow-up psychosocial and behavioral services. At Beach House Center for Recovery, for example, clients are encouraged to begin participating in these therapy and recovery groups as soon as possible, which can mean during medically supervised detox. And, as one scholarly overview of inpatient vs. outpatient detoxification clarified, “it is important that these interventions be introduced as quickly as possible” (to allow for the best chances of long-term recovery).
24/7 Supervision
Another benefit of inpatient rehab is the 24/7, medical and clinical supervision that a residential setting offers. For many people in early recovery, especially those suffering from a severe addiction, that supervision can be essential. The following criteria for inpatient alcohol detox can be a helpful guideline regarding who most stands to benefit from this feature of inpatient rehab:
- Those who lack a network of support
- Those who are experiencing moderate to severe withdrawal symptoms and/or have a known history of delirium tremens, alcohol withdrawal seizures or other severe drug withdrawal reactions
- Those at imminent risk of self-harm
- Those who have made multiple past attempts at treatment and/or undergone multiple detoxifications
- Those with a co-occurring disorder or who are in active psychosis or have suffered serious cognitive impairment
- Those who are unlikely to complete a supervised outpatient detox
- Those who are pregnant
Intensity of care
The intensity of care is yet another evidence-based benefit of inpatient rehab. Data-backed recommendations that appear in the “Treatment Protocol Effectiveness Study” (cited earlier) list “intensity of care” as a hallmark of much-needed improvements to substance abuse treatment. A residential inpatient setting is best positioned to provide that intensity of care associated with better recovery outcomes. For those seeking a structured, intensive level of care without requiring 24/7 residential support, a Partial Hospitalization Program (PHP) can serve as a highly effective alternative.
A supportive community of residential peers
Unlike outpatient settings, inpatient rehab allows clients to live in a residential community and to develop safe and supportive peer relationships that, research has shown, can be a critical ingredient in positive recovery outcomes. One evidence-based example here are therapeutic communities or structured, drug-free environments in which people in recovery live with one another during a period of extended, long-term residential treatment—and therapeutic communities and their strong peer community component have evidenced better outcomes. While many inpatient programs involve shorter lengths of stay than therapeutic communities, they share the same residential peer community feature that is linked with better outcomes.
The absence of former triggers
Addiction triggers can be especially troublesome during early recovery, be they a high-stress job environment, proximity to drug-using friends, or the liquor store next door. An inpatient setting safely removes clients from these high-risk factors for relapse, thereby lengthening their period of abstinence—and extended abstinence is a good predictor of long-term recovery, research has shown.
Higher treatment completion rates
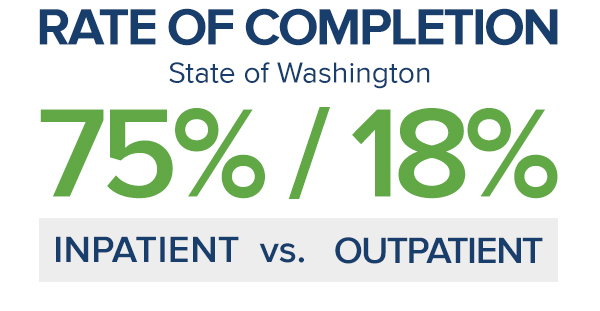
Finally, inpatient rehab correlates with higher treatment completion rates, which tend to be linked with better recovery outcomes. A study of clients discharged from drug and alcohol treatment programs in the state of Washington found a significantly higher rate of completion among inpatients (75 percent) versus intensive outpatients (18 percent), for example.
READY ACCESS TO EVIDENCE-BASED TREATMENTS
It is not enough to simply detox from drugs and alcohol in order to remain abstinent. Without becoming engaged in treatment, the now-sober individual is merely going through the motions. Inpatient rehab provides those who truly desire to live drug-and alcohol-free with ready access to evidence-based treatments, such as behavioral therapies, that may increase the likelihood that they’ll learn how to change their attitudes toward substance use and practice and begin healthier behaviors targeted toward sustaining abstinence following treatment.
Behavioral treatments are provided by psychiatrists, psychologists, social workers (with either Master of Social Work degree or a licensed clinical social worker), and alcohol and drug counselors (with appropriate state-required certification, as required).
Some of these behavioral therapies offered during multi-layered treatment may include:
Cognitive Behavioral Therapy (CBT)
Originally developed as a way to help those with alcohol abuse problems prevent relapse, cognitive behavioral therapy (CBT) was later modified to help cocaine-addicted individuals avoid relapse. CBT is based on the theory that learning processes are integral to developing the ability to identify and correct the kind of behavior that led to substance abuse, and to practice and become comfortable with strategies to effectively cope with triggers, cravings, high-risk situations and former drug- and alcohol-using friends.
Contingency Management (CM)
In essence, contingency management (CM) is a treatment strategy that involves providing incentives to clients diagnosed with alcohol use disorder (AUD) and other alcohol and other drug disorders (AOD) to reinforce compliance with prescribed medication and treatment attendance for alcohol and drug use. It may be part of a comprehensive treatment plan for the inpatient rehab client that includes other interventions of a psychosocial and/or pharmacological nature.
Mindfulness-Based Cognitive Therapy (MBCT)
Another treatment strategy that may be offered as part of a comprehensive inpatient drug and alcohol rehab treatment plan is mindfulness-based cognitive therapy (MBCT). Indeed, the use of mindfulness meditation for substance abuse treatment is, according to a 2009 article in Substance Abuse is a promising field of research with compelling evidence for its potential utility.
Motivational Enhancement Therapy (MET)
Addiction is a complex brain disorder that changes the way people think and act. Driven by cravings and urges as a result of these brain changes, the now-sober addict still has residual trace memory and leanings toward his or her substance of choice, both as a means of coping with stress and easing pain. The path to abstinence and recovery requires learning how make internally motivated behavior changes. Motivational enhancement therapy (MET) seeks to identify what needs to be changed and helps the client change their thoughts and behaviors about drug use, and set meaningful goals that reinforce a commitment to sobriety.
Acceptance and Commitment Therapy (ACT)
A psychotherapeutic approach to drug addiction treatment, acceptance and commitment therapy (ACT) is a subset of mindfulness-based therapies. ACT helps recovering addicts step back from their thoughts and stop negative and automatic reactions to people, places and things associated with their addiction.
Dialectical Behavior Therapy (DBT)
Many addicts entering inpatient rehab also have a co-occurring mental health condition that requires addressing along with SUD treatment. Originally developed to help those diagnosed with borderline personality disorder and chronic suicidal thoughts, dialectical behavior therapy (DBT) has evolved and been modified to treat a number of different mental health illnesses. With CBT as a core, DBT focuses on acceptance and validation of, instead of struggling with, uncomfortable thoughts, feelings and behaviors. Therapy then helps the client develop new skills, coping mechanisms and healthier behaviors to facilitate change and produce long-lasting improvement.
Family Behavior Therapy
Addiction is a disease that affects more than just the person diagnosed with the condition. Addiction affects everyone in the family. As such, while the addicted individual is benefitting from inpatient rehab, family members also can take advantage of family behavior therapy so they’re better able to support their loved one’s return home following treatment.
Interpersonal Therapy
An empirically-validated treatment intervention, interpersonal therapy, also called interpersonal psychotherapy, focuses on resolving problems associated with substance use. Once the primary interpersonal problem(s) are identified, targeted therapy seeks to help resolve the problems and helps the client take responsibility for and change his or her behaviors.
12-Step Facilitation
Participation in 12-Step meetings is highly recommended by addiction recovery experts as an essential component of an effective support network for the newly sober individual following completion of an alcohol and drug treatment program. Most residential rehab facilities introduce their clients to 12-Step groups, such as Alcoholics Anonymous, during treatment stay so they can become familiar with the group dynamic and how such self-help groups help members remain sober.
PREPARATION OF A RELAPSE PREVENTION PLAN
A key aspect of inpatient drug and alcohol rehab is preparing clients to return home following treatment with a well-defined relapse prevention plan. As the near-final step in the residential rehab stay, the client works with counselors to create a workable plan that can be modified according to changing needs to address the stressors and triggering situations likely to be encountered after treatment.
Components of the relapse prevention plan include:
- How to recognize triggers and cues that precipitate resumed alcohol or drug use
- Practical tips for how to handle a craving to drink or use drugs
- Developing contingency plans for how to handle stressful situations
- What to do if the client slips or goes into full relapse
- A list of contacts to call for immediate support
Sources:
Alcohol, Research & Health. “Contingency Management: Incentives for Sobriety.” Retrieved June 26, 2018.
National Alliance on Mental Illness. “Psychotherapy. Dialectical Behavior Therapy (DBT).” Retrieved June 27, 2018.
National Center for Biotechnology Information. “A Guide to Substance Abuse Services for Primary Care Clinicians. Chapter 5 – Specialized Substance Abuse Treatment Programs.” Retrieved June 21, 2018.
National Center for Biotechnology Information. “Substance Abuse and Family Therapy.” Retrieved June 27, 2018.
National Institute on Alcohol Abuse and Alcoholism. “Treatment for Alcohol Problems – Finding and Getting Help. Types of Professionals Involved in Care.” Retrieved June 25, 2018.
National Institute on Drug Abuse. “Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition). Behavioral Therapies.” Retrieved June 25, 2018.
National Institute on Drug Abuse. “Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition). Cognitive-Behavioral Therapy (Alcohol, Marijuana, Cocaine, Methamphetamine, Nicotine).” Retrieved June 25, 2018.
Substance Abuse. “Mindfulness-Based Therapies for Substance Use Disorders: Part 1 (Editorial).” Retrieved June 26, 2018.
Related Articles:
Benefits to Referring a Patient to an Offsite Drug or Alcohol Rehab







