Synthetic Drugs Detox Guide: Withdrawal Symptoms & Timeline
[three-fifths-first]
Synthetic drugs are an increasingly popular category of addictive substances derived from chemical compounds. Illicitly manufactured by “street chemists” using technically legal chemicals, they are considered far riskier than naturally sourced drugs. Comprised of over 200 different compounds, these highly profitable “designer drugs” are easy to purchase and readily available in a variety of legal and underground markets. Users frequently have no idea what is in the drug or how the suspiciously manufactured chemicals—often mass-produced in Chinese labs—will react to each other.
Synthetic drugs replicate the effects of plant-derived drugs like marijuana and cocaine, but are known for being highly addictive and dangerously unpredictable. Due to their volatility and the unknown side effects associated with use, synthetic drugs represent an emerging public enemy, challenging authorities to crack down on their production, distribution and use.
[/three-fifths-first]
[two-fifths]
TABLE OF CONTENTS
- Introduction to Synthetic Drugs Detox
- Synthetic Drugs Withdrawal Symptoms
- Synthetic Drugs Withdrawal Timeline
- Inpatient Treatment for Synthetic Drugs
- Outpatient Treatment for Synthetic Drugs
- Can Synthetic Drugs Detox Be Done at Home?
- Tapered vs. Cold Turkey
- Considerations for Synthetic Drugs Detox
- Recovery Success and Aftercare Services for Synthetic Drugs
[/two-fifths][clearfix]
Popular designer drugs include the following:
- Cannabinoids “K2” or “Spice,” psycho-actives made using lab-manufactured THC –the mind-altering substance found in cannabis—and known to be 50-100 times more potent than morphine
- Synthetic opiates Fentanyl and Krokodil, which mimic the effects of heroin and morphine
- The hallucinogen “N-Bomb” or “Smiles,” which is sold as a cheap alternative to LSD
- Flakka “bath salts,” a cathinone that produces the stimulant effects associated with cocaine and methamphetamine
Is synthetic drugs ruining your life? Call: (855) 935-2871
SYNTHETIC DRUG WITHDRAWAL SYMPTOMS
Synthetic drugs are most often abused by physically and psychologically vulnerable 12-17 year olds and not beholden to Food and Drug Administration (FDA) required manufacturing standards. The treacherously high potency of synthetic drugs, combined with their unpredictable reactions, makes withdrawal symptoms and the withdrawal process itself difficult to establish. (Obviously, high doses of the illicit stimulant Flakka will produce a different severity and variety of symptoms than low doses of a pharmaceutically-derived opiate like fentanyl.)
Even mild recreational users risk suffering horrific withdrawal symptoms, with the majority requiring enrollment in a medically managed detox program in order to safely recover. Upon admission into an inpatient detox program, a variety of clinical tools are used to establish symptoms based on quantifiable scores. One such assessment, the Clinical Opiate Withdrawal Scale (COWS), provides a reliable method for guiding Medication-assisted treatment (MAT) and helping clinicians select appropriate therapeutic interventions. The following cluster of symptoms may appear, depending upon the variety of synthetic drug as well as frequency, intensity and duration of use:
[one-half-first]
- Psychosis
- Tremors
- Chest pain
- Blurred vision
- Heart palpitations
- Coma
- Dehydration
- Vomiting
- Diarrhea
- Seizures
- Heart attack
[/one-half-first][one-half]
- Dizziness
- Difficulty breathing
- Chills/hot flashes
- Numbness
- Insomnia
- Paranoia
- Sweating
- Disorientation
- Stroke
- Sudden death
[/one-half][clearfix]
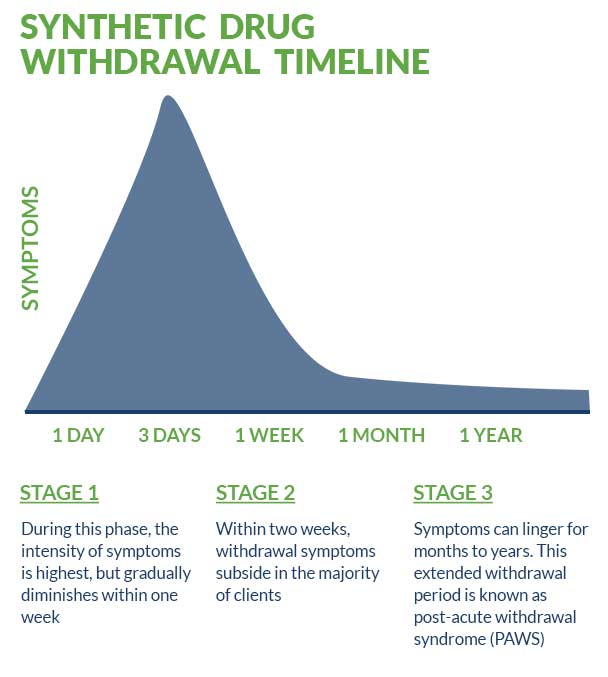
SYNTHETIC DRUG WITHDRAWAL TIMELINE
Synthetic drug withdrawal timelines, like withdrawal symptoms, are highly variable and difficult to establish. Typically, in cases of mild to moderate use, the acute phase of withdrawal peaks and subsides very quickly, within three to four days. During this phase, the intensity of symptoms is highest, but gradually diminishes within one week. Within two weeks, withdrawal symptoms subside in the majority of clients; however, they can linger for months and even years. This extended withdrawal period is known as post-acute withdrawal syndrome (PAWS) and may be severe enough that ongoing medication management and formal treatment are required in order to avoid relapse and other serious, debilitating consequences.
The half-life and extended life of various synthetic drugs are too variable to quantify, but tend to follow similar guidelines compared to other potent opiates. Although urine, blood and saliva samples may detect the substances within hours or days following use, hair samples are usually detectable for up to 90 days afterwards.
INPATIENT TREATMENT FOR SYNTHETIC DRUGS
Inpatient treatment is a highly popular, evidence-based protocol in which clients live at a designated facility— usually for a month, but in some cases, as many as three. During their stay, clients receive intensive medical supervision and ongoing medication management by a team of highly qualified professionals in addition to psychotherapy by licensed clinicians. Widely considered the industry “gold-standard” for effective treatment, intensive inpatient is an excellent choice for synthetic drug users—all of whom benefit from the 24/7 staff monitoring, heightened security, enhanced camaraderie and impressive ancillary services and benefits.
Medication-Assisted Treatment
Medication-assisted treatment (MAT) is an integral aspect of inpatient treatment that involves carefully administered doses of Food and Drug Administration (FDA) approved medications in tandem with psychotherapy. Cognitive behavioral therapy (CBT), motivational interviewing (MI), trauma-informed therapy, family therapy, and dialectical behavioral therapy (DBT) are all popular, evidence-based therapies included in the scope of MAT.
Depending upon the severity and type of synthetic drug abused—medications like Suboxone, Subutex and Vivitrol may be used to reduce the intensity of cravings and manage withdrawal symptoms. Antipsychotics are also used to treat cases of acute psychosis triggered by withdrawal from psychoactive “Spice,” a phenomenon known as “spiceophrenia.” In cases where extreme anxiety is the primary symptom, benzodiazepines “benzos” may be included in the treatment regimen.
Dual Diagnosis Treatment
A broad range of anxiety, depression and trauma-related disorders are known to be precipitating factors involved in synthetic drug addiction— and addiction in general. Treating these co-existing disorders is a critical aspect of inpatient treatment and supplemental medications include:
- Gabapentin
- Pregabalin
- Buspirone
- SSRIs
OUTPATIENT TREATMENT FOR SYNTHETIC DRUGS
Outpatient facilities allow clients to live at home while receiving treatment services, and provide the primary advantage of flexibility for clients whose personal and/or professional schedules require it. Offered in varying levels, certain facilities require a minimum commitment of five days per week while others require only one to two days per week, often during evening sessions. Generally cheaper than inpatient treatment, outpatient treatment is also considered less effective.
CAN SYNTHETIC DRUG DETOX BE DONE AT HOME?
- Self-guided, at-home synthetic drug detox is never recommended under any circumstance and may lead to potentially deadly consequences.
- Unfavorable treatment outcomes invariably follow self-treatment, including increased likelihood of future relapse, heightened withdrawal symptoms and debilitating psychological effects.
TAPERED VS COLD TURKEY
“Cold turkey” refers to abrupt discontinuation of use. Quitting any medication cold turkey is never recommended and may lead to a frightening, unpredictable acceleration and intensification of symptoms called “precipitated withdrawal.” Preventing precipitated withdrawal is the primary goal of medically supervised detox. “Tapering” describes a practice that involves administering carefully controlled doses of a drug to help wean the user off. Tapering has been deemed unnecessarily risky, with mounting evidence supporting the efficacy of stabilizing medications like Suboxone, Subutex and Vivitrol— especially when treating highly potent synthetic drugs like fentanyl.
CONSIDERATIONS/ HOW TO DECIDE WHAT IS RIGHT FOR YOU
For the majority of clients, the decision to enroll in treatment will depend upon insurance coverage, affordability, location and reputation. Reputable facilities will be able to verify insurance benefits prior to enrollment. In cases where partial, if not total, coverage is denied, additional options (grants, scholarships or affordable payment plans) may be available.
RECOVERY SUCCESS AND AFTERCARE SERVICES FOR SYNTHETIC DRUGS
Successful completion of inpatient detox is only the beginning of the recovery journey. A comprehensive relapse prevention plan should include the following aftercare support services—all of which are empirically-proven to increase favorable treatment outcomes:
- 12-step involvement (NA and AA)
- Sponsorship
- Random drug testing
- Life and job skills coaching (as needed)
- One-on-one and/ or group therapy
- Sober peer support
- Avoidance of environmental triggers
- Ongoing medication management
For more about synthetic drug detox and recovery, check out these related articles:
- Synthetic Drug Detox: What to Expect
- The Dangers of Drug Detox at Home and Quitting Cold Turkey
- Synthetic Drugs: Addiction and Treatment
- Why Early Intervention for Addiction Is Critical
- Understanding the Dangers of Designer Drugs
Is synthetic drugs ruining your life? Get help now
[expand title=" Sources:" targclass="highlight"]
International Journal of Neuropsychopharmacology. Spice/K2 drugs—more than innocent substitutes for marijuana. March, 2014.
National Institute on Drug Abuse (NIDA). Synthetic Cannabinoids. Feb, 2018.
Pharmacy and Therapeutics. Synthetic Cathinones (‘Bath Salts’). Oct, 2012.
Policing and Society. Networks and Meta-regulation: Strategies Aimed at Governing Illicit Synthetic Drugs. Nov, 2006.
Frontiers in Psychiatry. Synthetic Cathinone and Cannabinoid Designer Drugs Pose a Major Risk for Public Health. August, 2017.
The New England Journal of Medicine. “Bath Salts” Intoxication. September, 2011.
Science. Underground labs in China are devising potent new opiates faster than authorities can respond. March, 2017.
[/expand]